Exercise, Inflammation, and Immune System Interactions: An Integrated Perspective
Exercise serves a multifaceted role in the body, particularly concerning inflammation and immune responses. Regular physical activity is documented to reduce chronic inflammation, contributing to overall well-being. Studies show that exercise promotes the release of anti-inflammatory cytokines and decreases the levels of pro-inflammatory markers in the bloodstream. This effect can translate into better health outcomes for individuals suffering from various chronic conditions, such as cardiovascular disease, obesity, and autoimmune disorders. A comprehensive understanding of the interaction between exercise and inflammation can inform therapeutic approaches for managing inflammation-related diseases. Exercise-induced improvement of oxidative stress and modulation of immune cell activity indicates a complex relationship that merits further exploration. Furthermore, when investigating these processes, researchers often focus on the specific modalities of exercise such as aerobic versus resistance training and their differential impacts on inflammation markers. By employing tailored exercise regimens, individuals may experience beneficial adaptations that support immune function and reduce inflammation. Thus, exploring the integrated perspective of exercise’s effects on inflammation and immune mechanisms becomes increasingly important for both practitioners and individuals striving for better health. Contextualizing research findings within practical applications enhances the relevance of these insights in everyday life.
The Role of Inflammation
Inflammation is a natural and essential process in response to injury or infection, acting as the body’s defense mechanism. However, chronic inflammation can lead to detrimental health effects and is implicated in various diseases. Understanding how exercise influences inflammation allows researchers and practitioners to develop strategies to mitigate these adverse effects. For instance, regular physical activity is shown to decrease levels of inflammatory markers, such as C-reactive protein (CRP) and interleukins. Moreover, certain types of exercise, like aerobic training, have demonstrated effectiveness in reducing systemic inflammation. Conversely, excessive exercise without adequate recovery can contribute to increased inflammation, emphasizing the need for a balanced approach. It becomes imperative to identify an individualized exercise plan that factors in the person’s baseline health status, fitness level, and inflammatory conditions. Addressing these individualized factors helps optimize health benefits while minimizing the risks of exacerbating inflammation. Understanding personalized exercise protocols that suit various populations can lead to lasting changes in health outcomes, facilitating personalized medicine’s goals. Engaging in this discourse surrounding exercise and inflammation fosters a greater understanding of achieving optimal health through lifestyle modification.
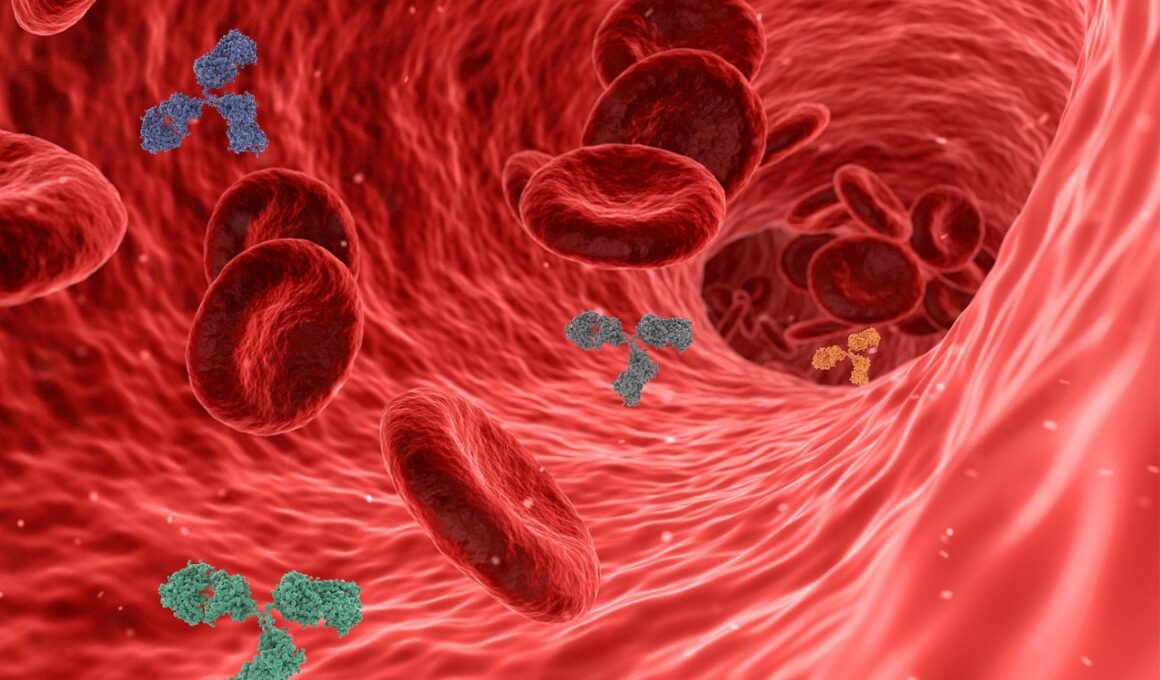
The immune system plays a critical role in mediating inflammation, as it identifies and responds to pathogens and injuries. Regular exercise has been associated with a more robust immune response. However, understanding the delicate balance between exercise intensity, duration, and the body’s immune function is essential. Moderate exercise enhances the circulation of immune cells, including lymphocytes and neutrophils, increasing their effectiveness in combating potential infections. Such benefits have been substantiated by research indicating that physically active individuals experience fewer incidences of viral infections, notably respiratory illnesses. In contrast, high-intensity and prolonged exercise can temporarily suppress the immune system, leading to a state known as the “open window” theory, which increases susceptibility to illness. Strategies that promote recovery, such as proper hydration and nutrition, become vital in maintaining a balanced immune function. Therefore, it is essential for both athletes and non-athletes to identify their limits regarding exercise intensity and to prioritize recovery. Emphasizing the relationship between exercise and immune response can assist individuals in achieving a lifestyle that fosters resilience and health while minimizing the risk of undue inflammation and immune dysregulation.
The type of exercise performed can have distinct effects on inflammation and immune responses. Aerobic exercise, such as brisk walking, swimming, or cycling, has consistently shown beneficial effects in mitigating inflammation. These activities can increase blood circulation, enhance oxygen delivery, and promote the clearance of metabolic waste. On the contrary, resistance training is effective in building muscle strength and mass, which also has implications for modulating inflammation. Studies suggest that a combination of both aerobic and resistance training is optimal for improving overall health and diminishing chronic inflammation. Moreover, high-intensity interval training (HIIT) has emerged as a popular exercise modality, known for its efficiency and effectiveness. HIIT can provoke a significant acute inflammatory response, stimulating the body to adapt positively. Engaging in diverse exercise forms fosters improved functional capacity and encourages adherence by providing variety, contributing to long-term lifestyle changes. Incorporating different intensities and types of exercise not only promotes physical health but also mental well-being. This diversity within an activity repertoire allows individuals to find enjoyment, further enhancing motivation toward maintaining an active lifestyle.
Nutrition plays an equally significant role alongside exercise in managing inflammation. The food we consume can dictate the body’s inflammatory response, interacting with the immune system directly. Diets rich in fruits, vegetables, whole grains, and healthy fats have anti-inflammatory properties and complement the effects of exercise. Omega-3 fatty acids, found in fish and flaxseeds, are particularly notable for their role in reducing inflammation. A balanced diet can amplify the positive effects of regular exercise, creating synergy that promotes overall health. Conversely, diets high in added sugars and processed foods can exacerbate inflammation and counteract the benefits of physical activity. Understanding the interaction between nutrition, exercise, and inflammation underscores the importance of adopting a holistic approach towards health. Individuals seeking to reduce inflammation should consider both the quantity and quality of their food intake as part of their comprehensive strategy. Furthermore, educating individuals about nutrition’s role in conjunction with exercise can enhance their capability to make informed dietary choices that support immune function. Emphasizing nutrition and exercise together fosters better health outcomes and establishes lasting lifestyle habits aimed at managing inflammation effectively.
Chronic stress can influence inflammation and immune function, interacting with exercise’s effects. Stress triggers the release of cortisol, a hormone that can suppress immunity and promote inflammation when persistently elevated. Incorporating stress management strategies along with regular exercise may yield significant health benefits. Mindfulness practices, such as yoga or meditation, combined with physical activity, can help regulate the stress response while promoting relaxation. These techniques reduce cortisol levels and enhance overall well-being, offering a comprehensive strategy to combat chronic inflammation. Engaging in outdoor activities or exercising in nature can further elevate mood and mitigate stress. Creating an environment that promotes emotional health, alongside physical fitness, enables individuals to foster resilience against stress-induced inflammation. By recognizing the interplay between stress, exercise, and inflammation, health professionals can devise multidisciplinary approaches. Integrating mental health strategies with physical fitness programs creates a more profound impact on individuals’ overall health. Encouraging individuals to view exercise as a means of stress relief can enhance adherence to fitness regimens, fostering lifelong healthy habits. Cultivating this awareness can empower individuals to take control of their health, improving their quality of life as they navigate challenges.
In summary, the interactions between exercise, inflammation, and immune function are intricate and critical to healthy living. Regular physical activity has undeniable advantages in reducing chronic inflammation and improving immune responses, positively influencing various health outcomes. Emphasizing individualized exercise regimens, understanding the role of nutrition, addressing stress, and embracing diversity in physical activities is essential in maximizing these benefits. Education and awareness around these topics can empower individuals to embrace lifestyle changes, enhancing physical and mental health. Through continuous research, practitioners can translate scientific insights into effective public health initiatives aimed at minimizing inflammation-related diseases. Fostering community programs that promote physical activity and education about inflammation can extend far-reaching effects. Researchers must also seek to explore the underlying biological mechanisms associating exercise with immune function further. As knowledge expands, health professionals can refine strategies to support populations facing chronic inflammation, including tailored fitness programs. Integrating these aspects into a cohesive approach amplifies health promotion efforts. In navigating the complexities of exercise science, prioritizing inflammation management alongside immune health paves the way for healthier societies and improved quality of life for all individuals.