Understanding Hydration in Elderly Populations
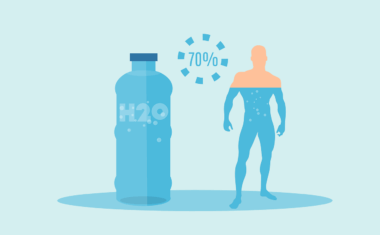
Proper hydration is a critical yet often overlooked aspect of health, especially in elderly populations. Many older adults face challenges that can lead to dehydration, including decreased thirst perception, changes in kidney function, and certain medical conditions. As age advances, the body’s ability to conserve water diminishes, making regular fluid intake essential. Dehydration increases the risk of urinary tract infections, confusions, and even hospitalization. Maintaining optimal hydration supports various bodily functions, such as temperature regulation and joint lubrication, while also aiding in digestion. It is crucial for elderly individuals to recognize their fluid intake needs. In addition, caregivers should monitor hydration levels and encourage fluid consumption regularly. Simple strategies, such as drinking water at meals or having fluids readily available, can help. Foods with high water content, like fruits and vegetables, can also contribute to hydration. Furthermore, understanding medications that may affect fluid balance is essential. Thus, the importance of hydration cannot be understated, making it a priority for the health of elderly individuals in our society.
Impact of Dehydration on Body Composition
Dehydration significantly affects body composition, particularly among elderly individuals who may struggle more with fluid balance. When the body lacks sufficient water, it may lead to altered body weight and an increase in body fat percentage due to decreased intracellular fluid. Lower hydration levels can result in a skewed analysis of body composition, creating misconceptions about an individual’s overall health status. Fluid loss also impacts muscle mass, which is especially crucial for seniors aiming to maintain mobility and independence. Muscle tissue is highly water-dense, so a decrease in water intake can lead to a decline in muscle function and strength. This situation creates a vicious cycle; as seniors lose muscle mass, their physical activity levels often decrease, further exacerbating hydration issues. Understanding these connections emphasizes the importance of staying hydrated to preserve muscle and fat distribution. Therefore, assessments of hydration status must be integrated into discussions about body composition in older adults. Encouraging regular hydration can mitigate the adverse effects of dehydration on body composition, promoting better overall health outcomes.
In addition to hydration’s impact on body composition, the relationship between fluid intake and dietary habits warrants attention among elderly populations. Many older adults tend to consume fewer fluids due to altered taste sensitivity. Consequently, they may consume less of essential beverages. This deficiency could lead to inadequate hydration levels while perpetuating poor nutritional choices. Additionally, older adults frequently experience changes in their appetite or difficulty eating, which contributes to their overall fluid intake. By enhancing the sensory aspects of food and drinks, caregivers and family members can encourage higher fluid consumption. Flavoring water with fruits or incorporating soups into meals are effective methods to increase hydration. Ideally, seniors should aim for a minimum daily fluid intake, which can vary depending on activity levels and health conditions. Hydration should be viewed as part of a comprehensive diet, where appropriate education on dietary choices supports adequate fluid and nutritional intake. Raising awareness of hydration’s significance can positively influence health, resilience, and longevity, nurturing a healthier aging process for seniors and ultimately creating improved quality-of-life outcomes.
Evaluating Hydration Status
To ensure the elderly maintain adequate hydration, assessing hydration status becomes crucial. There are various techniques to evaluate an individual’s hydration, including observing physical signs and symptoms. Common indicators involve tracking urine color, frequency, and overall volume, which can reveal potential dehydration levels. Moreover, senior care professionals may utilize more advanced methods, such as bioelectrical impedance analysis or skin turgor tests. By considering these approaches, caregivers can better tailor hydration strategies to individual needs. Another important aspect to consider is the influence of medications, as certain drugs can cause side effects that exacerbate fluid loss or hinder fluid intake. Professionals should remain vigilant regarding medications that impact hydration and work collaboratively with healthcare providers to modify treatment plans where necessary. Community awareness programs can educate family members about recognizing dehydration signs to help combat the issue more effectively. Proper education on hydration should be an integral part of educational outreach, targeting seniors and those caring for them. Keeping the elderly well-hydrated greatly enhances their physical well-being and cognitive function, thus fostering healthier aging.
With technology increasingly embracing the health management space, wearable devices have the potential to play a significant role in monitoring hydration. These gadgets can track physical activity, providing insights into how much fluid seniors need to remain hydrated. Moreover, using smartphone applications can offer reminders to drink water and help track daily intake. This incorporation of modern technology can aid in addressing hydration gaps faced by older adults. Additionally, telehealth platforms can facilitate discussions regarding hydration and nutrition, ensuring elderly patients remain engaged in their health management. Resource accessibility can empower seniors and caregivers with the necessary tools to enhance hydration awareness and practices. Social support systems, including family, friends, and peers, moreover, can reinforce the importance of hydration. Fostering community-based programs that promote hydration awareness creates discourse around healthy habits and encourages involvement. Engaging older adults in discussions regarding their hydration needs leads to improved health outcomes and well-being. Ultimately, leveraging technological advancements in conjunction with social support strategies enriches the care and guidance available to seniors, enhancing overall hydration awareness.
Strategies for Promoting Hydration
Implementing effective strategies for promoting proper hydration within elderly communities is essential. Educating seniors about the importance of regular fluid intake is vital. Beyond education, creating an environment that encourages drinking can significantly boost hydration levels. Cultivating a culture that normalizes beverage consumption throughout the day, paired with easy access to fluids, fosters healthier habits. Caregivers should provide a variety of beverage options; offering flavored water, herbal teas, and low-sugar fruit juices increases choice and encourages hydration. Regular scheduling of fluid intake during meals, snacks, and even social activities can also improve fluid consumption. Another essential aspect is assessing individual preferences and needs to curate personalized hydration plans. For example, some seniors may prefer certain temperatures for drinks or specific types of beverages. Being attentive to these preferences can significantly enhance fluid intake. Furthermore, recognizing the signs of dehydration early on can prompt timely interventions. Maintaining hydration charts at senior care facilities or during home visits allows caregivers to track intake and adjust strategies accordingly. As a result, enhancing hydration among the elderly not only improves well-being but also empowers them to remain active and engaged.
Ultimately, increasing awareness about hydration’s importance within body composition analysis in elderly populations can lead to improved health outcomes. Understanding hydration levels allows for more accurate assessments of body composition and encourages conversations surrounding effective health management. By partnering with healthcare providers, caregivers, and family members, seniors can prioritize hydration as a key component of their overall health strategies. Healthy hydration habits can be cultivated through education, support, and empowering tools that make drinking fluids easier. Moreover, encouraging community engagement surrounding hydration can foster connections and shared resources among seniors. When seniors are more informed regarding their hydration needs and practices, they are likely to take an active role in their health management. Enhanced hydration knowledge ultimately leads to the preservation of physical and cognitive functions, enabling healthier aging experiences. Continuous research is crucial, as findings may lead to better strategies tailored for the aging population regarding hydration and body composition analysis. In conclusion, proper hydration serves as a foundational pillar of health that significantly enhances quality of life for the elderly community.
In summary, addressing hydration considerations in elderly populations showcases the need for comprehensive strategies that foster awareness, education, and action. With the prevalent risks of dehydration impacting body composition and overall health, we must prioritize hydration. Regular monitoring, simple interventions, and community awareness initiatives can collectively combat the common challenges faced by seniors. Caregivers play a fundamental role in supporting elderly individuals by implementing tailored strategies that meet their hydration needs. Moreover, fostering discussions surrounding hydration within individual and group settings paves the way for social support systems that further encourage consistent fluid intake. As we tackle the complexities of health management in aged populations, the importance of hydration must remain at the forefront. Staying informed and proactive in promoting hydration ultimately ensures that seniors can thrive in their daily lives. Emphasizing the connection between hydration and body composition further strengthens the case for proper fluid intake. In the end, embracing this understanding leads to improved health outcomes and enhanced life quality for the aging population.