Depression and Sleep: Breaking the Vicious Cycle
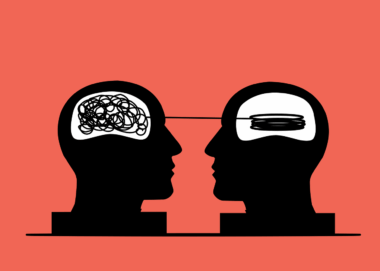
The relationship between sleep and mental health has garnered considerable attention, particularly concerning depression. Individuals suffering from depression often experience sleep disturbances, which can include insomnia or excessive sleepiness. These issues exacerbate feelings of fatigue, irritability, and difficulty concentrating. Poor sleep quality interferes with mood regulation and cognitive function, perpetuating the cycle of depression. This cyclical nature creates a challenging situation for individuals trying to recover. Not only can sleeplessness worsen existing depressive symptoms, but a lack of restorative sleep can also trigger new depressive episodes. Consequently, addressing sleep issues becomes paramount in the management of depression. By focusing on sleep quality, individuals can potentially experience improvements in their depressive symptoms. Behavioral and lifestyle changes that promote healthy sleep hygiene can significantly affect overall mental well-being. Simple measures, such as establishing a regular sleep schedule, practicing relaxation techniques, and minimizing screen time before bed, can foster better sleep habits. As awareness of this connection grows, both mental health professionals and individuals alike can benefit from strategies that support better sleep and, in turn, better mental health.
Research indicates that sleep problems, often a characteristic of depression, can lead to increased impulsivity, heightened emotional sensitivity, and a diminished capacity for stress management. Symptoms such as low energy and lack of motivation may additional impair daily functioning. A vicious cycle often emerges where sadness and anxiety hinder the ability to fall or stay asleep. This situation can become particularly concerning for those with concurrent mental health issues. Fortunately, there are multiple approaches to tackle this complex relationship. Therapeutic interventions like cognitive-behavioral therapy for insomnia (CBT-I) have shown promise in assisting patients with both depression and sleep-related issues. Furthermore, organizational techniques, mindfulness exercises, and even gentle physical activity may enhance sleep quality while addressing depressive symptoms. The key lies in developing a tailored approach that recognizes individual circumstances and unique patterns. By honoring the interconnected nature of sleep and mental health, it becomes possible to break free from this destructive loop. Recovery is entirely feasible, with commitment and support. Individuals can embark on a path leading toward better sleep, improved mood, and an overall higher quality of life.
Understanding the Science Behind Sleep and Depression
The connection between sleep and depression is profoundly rooted in biological mechanisms. Sleep disturbances can significantly affect neurotransmitters, including serotonin and dopamine, which play crucial roles in regulating mood. A lack of restorative sleep may disrupt these chemicals, causing or exacerbating feelings of sadness or hopelessness. Sleep, particularly REM sleep, is vital for emotional processing and memory consolidation. Insufficient REM sleep can lead to increased emotional dysregulation and difficulty managing stressors. In turn, heightened stress levels may lead to trouble sleeping, fostering a self-perpetuating cycle. Physiologically, sleep deprivation can alter cortisol levels, leading to increased anxiety, which can further interfere with sleep. Additionally, inflammation linked to poor sleep has been shown to correlate with depressive symptoms, creating a biological basis for these intertwined issues. As this intricate relationship becomes more comprehensive, interventions targeting sleep patterns may be more widely adopted in treating depression. Interventions can range from counseling and medication to lifestyle adjustments, tailored to each person’s unique needs. Fostering a healthy sleep environment may also enable individuals to break this vicious cycle and enhance their mental health.
The indirect effects of sleep on depression cannot be overlooked. Anxiety and chronic stress can emerge in individuals facing prolonged sleep issues, compounding feelings of despair. As these secondary symptoms materialize, individuals may find themselves caught in additional layers of mental health struggles. Factors such as caffeine intake, late-night electronic use, and irregular sleep schedules can significantly disrupt sleep cycles. Moreover, sleep apnea and other medical issues may also exacerbate challenges related to sleep hygiene. Addressing these root causes is essential for anyone seeking to break the sleep-depression cycle. Strategies like frequent sleep assessments, sleep logs, and open discussions with healthcare professionals can provide vital insights. These practices can promote awareness of sleep habits and their effects on mental health. Combating sleep issues as part of a holistic mental health strategy is paramount. Caregivers and individuals can work collaboratively to develop a treatment plan that accounts for sleep hygiene as foundational to overall emotional well-being. The recognition of sleep as a pivotal partner in mental health treatment is a crucial step in fostering resilience and nurturing recovery.
Strategies for Improving Sleep to Alleviate Depression
Implementing effective strategies to enhance sleep quality can be a game-changer for anyone dealing with depression. Establishing a consistent sleep schedule is one of the simplest yet most effective changes to make. Going to bed and waking up at the same time each day encourages the body’s natural circadian rhythms. Moreover, creating a relaxing bedtime routine plays an instrumental role in signaling the brain that it’s time to unwind. Activities like reading, meditating, or taking a warm bath can transition individuals into a state conducive to sleep. Additionally, ensuring that the sleep environment is comfortable—where the temperature is neither too hot nor too cold—can significantly affect sleep quality. Reducing light exposure and noise can further enhance restfulness, ensuring restorative sleep. Individuals may also benefit from journaling thoughts before bedtime to declutter the mind. Nutritional choices, such as avoiding heavy meals and stimulants close to bedtime, could contribute positively. By integrating these strategies into daily life, individuals can create a sustainable path toward better sleep and, consequently, improved mental health.
Engaging in regular physical activity can profoundly impact both sleep and mood. Exercise effectively decreases stress levels, releasing endorphins that uplift spirits. Integrating exercise into a daily routine can facilitate improved sleep patterns, leading to a more restorative night’s rest. However, timing is crucial; exercising too close to bedtime can hinder sleep. Finding an appropriate balance of activity and rest is essential for overall well-being. Another fundamental aspect to consider is nutrition. A balanced diet rich in vitamins and nutrients can support sleep quality and mental health. Omega-3 fatty acids, for example, have been linked to reduced depression symptoms, highlighting the connection between diet and emotional well-being. Furthermore, limiting alcohol and caffeine intake contributes to better sleep hygiene. Keeping a watchful eye on what goes into the body invites greater awareness of the potential impact on sleep and mental health. As individuals work toward optimizing their diets and lifestyles, they will uncover ways to foster a nurturing environment for both sleep and mental health recovery.
Seeking Professional Help for Sleep and Mental Health Issues
When self-help strategies do not yield the desired improvements, seeking professional assistance may best address intertwined sleep and depression. Mental health specialists can offer tailored treatments that address the unique challenges faced by individuals. Furthermore, they may recommend specialized therapies, medications, or referrals to sleep specialists. Engaging with professionals can provide holistic support, encompassing both mental and physical health needs. Therapies like cognitive-behavioral therapy for insomnia or mindfulness-based stress reduction can promote healthier sleep patterns. In some cases, pharmacological options may be necessary to stabilize chemical imbalances. Therefore, individuals must not hesitate to reach out for support and explore avenues for healing. Maintaining open communication with healthcare professionals about sleep patterns, mood changes, and concomitant issues is vital for establishing comprehensive care plans. Ultimately, combining clinical guidance with personal initiatives can maximize chances of overcoming challenges stemming from sleep and depression. By taking these crucial steps, individuals can pave their way toward recovery, mutual understanding, and improved quality of life. Empowerment through knowledge and expert support is ultimately the cornerstone of restoration.