Mythbusting: Can Fitness Cure Chronic Diseases?
Chronic diseases such as diabetes, heart disease, and arthritis are increasingly prevalent in today’s society. Many people believe that engaging in fitness activities can completely cure these conditions. This is a myth. While fitness can significantly improve health outcomes, it is crucial to understand that chronic diseases are complex and require comprehensive management. Regular physical activity can lead to better insulin sensitivity and weight management for diabetics, but it is not a stand-alone cure. Challenging myths is essential to avoid disappointment and to know the value of a multi-faceted approach in treatment. Combining fitness with medical advice, appropriate medications, and lifestyle changes will lead to optimal health. Furthermore, adherence to professional treatment plans is vital. Educating the public about these realities helps create realistic expectations regarding fitness and chronic disease management. It is advisable to consult healthcare professionals before commencing new fitness programs, as they can provide tailored advice and identify any specific risks. Aiming for gradual improvement through fitness is always a valuable goal and should not be overlooked in chronic disease management.
The importance of understanding the role of fitness in chronic disease management cannot be overstated. While fitness plays a vital role, it should not be viewed as a panacea for all health issues. This misconception can lead to individuals neglecting necessary medical treatments or relying solely on exercise to manage their conditions. Some common chronic diseases have specific requirements that fitness alone cannot fulfill. For instance, those with hypertension need medication and dietary interventions along with exercise. Similarly, individuals with arthritis may benefit from targeted strength training but need to avoid activities that exacerbate their condition. Thus, fitness should complement a more extensive treatment plan rather than replace it. Those who engage in exercise should focus on tailored fitness regimens that consider their specific health concerns. Physical activity can improve overall well-being, enhance mood, and reduce symptoms, but it’s crucial to embrace fitness as a supportive measure. When approaching chronic diseases, maintaining a holistic view will uplift individuals and encourage sustainable health practices overall, thereby enhancing quality of life and well-being for those affected.
It’s essential to differentiate between myths about fitness and facts surrounding chronic disease management. One prevalent myth suggests that simply engaging in fitness routines will erase the underlying causes of chronic diseases. Fitness, defined broadly as any form of physical activity, does have positive health effects. However, it alone is insufficient to eradicate health problems. This contrast is crucial for understanding how lifestyle modifications can contribute systemically. Failing to understand this distinction may lead individuals to take unnecessary risks, such as overstressing their bodies during exercise without accounting for their unique health statuses. Education is critical in mitigating myths surrounding chronic diseases. Increased understanding empowers individuals to take charge of their health through informed decisions about fitness and disease management. By focusing on complementary strategies that include medical guidance and proper fitness, individuals are more likely to achieve lasting health benefits. Staying informed about chronic disease and developing a balanced regimen will enable individuals to harness the power of fitness effectively. Ultimately, embracing this collective approach offers the best opportunity for long-term health improvements and fitness outcomes.
Evidence-Based Practices in Chronic Disease Management
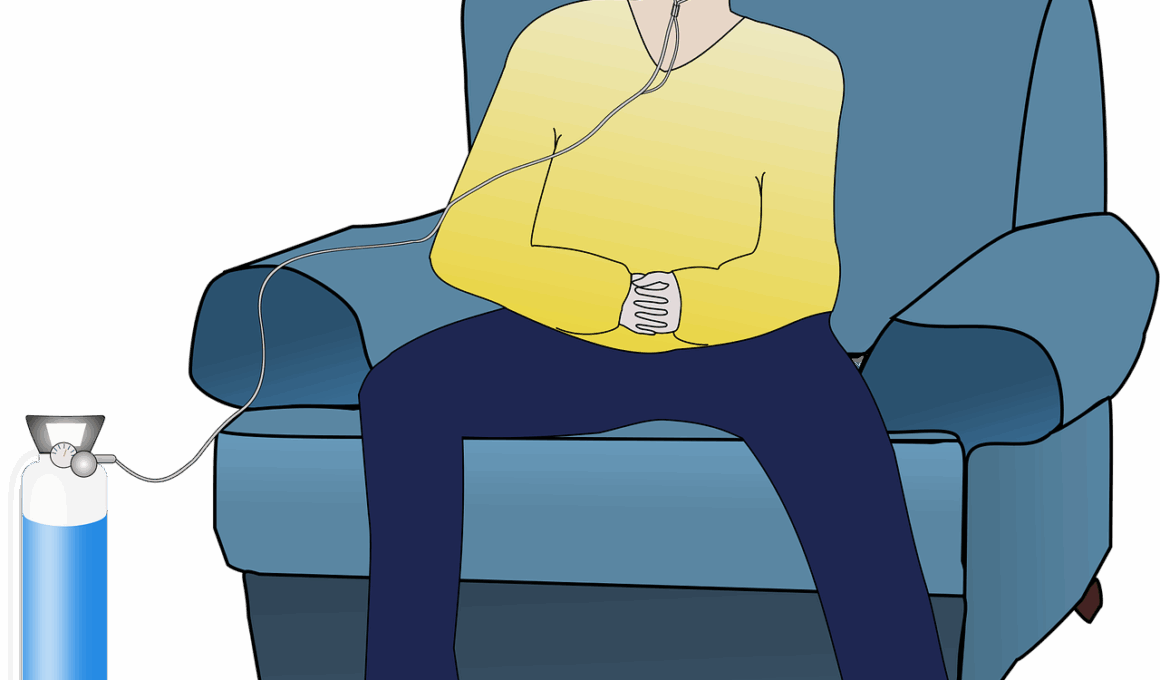
There’s a wealth of data supporting the integration of fitness into chronic disease management strategies. Several studies have shown that regular physical activity can decrease the impact of chronic illnesses on daily life, improve physical functioning, and enhance psychological well-being. For example, patients with chronic obstructive pulmonary disease (COPD) significantly improved their breathing and stamina through structured exercise programs, although medication remained essential. Likewise, individuals managing cardiovascular diseases showed noticeable benefits from consistent aerobic activities. Incorporating fitness into daily routines can provide immense health benefits, thus fostering better coping strategies against illness. Engaging in fitness activities can also encourage individuals to socialize, motivating them further in their recovery journeys. Group fitness classes, for example, can promote camaraderie and support, which is incredibly valuable for those facing chronic illnesses. However, it’s vital for these activities to be monitored by healthcare professionals. Hence, drawing knowledge from recent research strengthens confidence in adopting fitness as a part of chronic disease management plans and promotes a holistic viewpoint on patient health and well-being moving forward.
The fitness industry often promotes specific workouts as solutions to chronic diseases, which leads many to adopt these fads blindly. This oversimplified viewpoint is detrimental as it can funnel individuals into activities that might not suit their conditions. For instance, high-impact workouts may not be advisable for individuals with joint issues or osteoarthritis. Personalization is critical; tailored fitness programs are far more effective for managing chronic diseases. Consulting qualified trainers who understand chronic health conditions can significantly enhance safety and outcomes. It’s also primary for individuals to be educated about their limitations and work at their own pace without pressure. Implementing moderate-intensity workouts, durability training, and even gentle forms of exercise such as yoga can be effective. This personalized approach harmonizes fitness aspirations with practical health considerations, improving adherence to exercise routines, and optimization of results. Additionally, maintaining a watchful eye on advancements and new findings in chronic disease research helps individuals and trainers alike adjust programs accordingly. By prioritizing safety and effectiveness in fitness, individuals can achieve their health goals without jeopardizing their long-term well-being.
Conclusion: Embracing a Holistic Approach
In conclusion, while fitness plays a crucial role in managing chronic diseases, it should be approached with informed realism. Myths suggesting fitness can cure these diseases can lead to unmet expectations and misplaced priorities. This highlighting of facts versus fictions is crucial to foster healthy attitudes towards exercising with chronic illnesses. Individuals need to understand that combining physical activities with dietary changes, ongoing medical treatment, and lifestyle modifications presents the best pathway for health improvement. Fitness should never be perceived as a substitute for medical interventions; instead, it should be recognized as a powerful tool that works alongside existing treatments. By addressing chronic diseases through this multi-faceted perspective, individuals can achieve comprehensive health management goals. It’s essential to encourage continual learning about one’s condition and consult professionals when attempting new fitness endeavors. Seeking a supportive community, whether through clubs or online channels, can reinforce motivation and optimism for individuals on their health journeys. Ultimately, embracing a holistic approach allows individuals to thrive, ensuring that their aspirations for health and fitness are rooted in reality and understanding.
Last but not least, addressing misconceptions surrounding fitness and chronic diseases fosters an empowered mindset. This understanding equips individuals to advocate for themselves while navigating their health journeys. It’s equally important for healthcare providers to navigate conversations around fitness as part of disease management. Such engagements can help diminish stigma and provide clear guidance for patients exploring their fitness options. Dissemination of accurate, evidence-based information concerning the benefits and limitations of fitness will promote wellness and informed decision-making. Collaboration between fitness professionals and healthcare providers promotes an empathetic framework that nurtures overall patient health. Both communities should strive to support chronic patients in finding the best paths forward via exercise while ensuring safety and consideration for their specific health contexts. To conclude, genuine optimism about the role of fitness in chronic disease management goes a long way, enhancing both engagement and support. When centered on enduring health outcomes, both patients and professionals can work collectively to build and shape these narratives, establishing a healthier tomorrow for everyone involved.
To summarize, understanding that fitness is a piece of the puzzle in chronic disease management is critical. It aids in recognizing that while exercise yields benefits, it also warrants the support of comprehensive medical guidance and healthy lifestyle choices in managing long-term conditions. Fitness should not be pursued in isolation, as that would defeat the purpose of its incorporation into holistic health management plans. Embracing multi-disciplinary approaches not only amplifies individual health outcomes but also fosters healthier communities. Therefore, promoting accurate narratives regarding exercise adherences through regular communication and outreach will pave the way for improved health perspectives. The ultimate goal is healthy living, which can only be achieved through collaboration, proper education, and understanding the role each component plays. As individuals adapt to varying challenges, maintaining balance and clarity in health-related decisions ensures they remain focused and feel empowered on their journeys through chronic disease management. Cultivating a supportive environment, guided by compassionate professionals, can create a culture of understanding that facilitates improved health, optimism, and resilience in those affected. This transformational approach breathes life into meaningful engagement and connection among communities tackling chronic diseases.