The Prognostic Value of Body Composition in Chronic Disease Outcomes
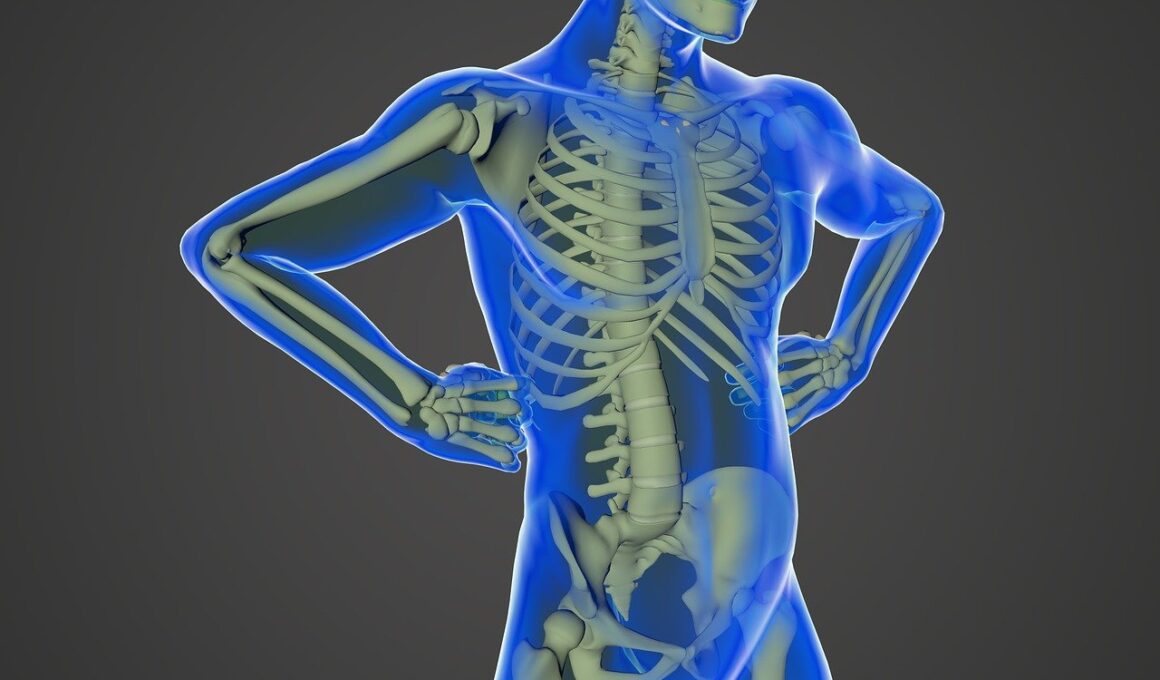
Understanding body composition is vital in assessing health outcomes, especially in chronic diseases. Body composition refers not just to weight but also to the makeup of fat, muscle, and bone. These measures can indicate the state of one’s health. Research shows that body composition can help predict the progression of chronic diseases like diabetes, heart disease, and even cancer. By evaluating the distribution of fat and lean mass, healthcare professionals can identify those at risk of complications and tailor interventions accordingly. Accurate measurements can facilitate better clinical decision-making. For instance, patients with excess visceral fat, more dangerous than subcutaneous fat, may have different therapeutic needs. Additionally, monitoring changes in body composition can signal an improvement or deterioration in health, making it a key factor in longitudinal studies. Various techniques, like bioelectrical impedance analysis, dual-energy x-ray absorptiometry, and magnetic resonance imaging, offer insights into body composition. Understanding the prognostic significance of these measurements might become critical for effective management of chronic diseases, ultimately improving patient outcomes and quality of life.
Role of Fat Distribution in Disease Prognosis
The distribution of body fat plays a significant role in predicting disease outcomes. Visceral fat, located around the organs, is linked to a heightened risk of numerous chronic illnesses. Studies indicate that patients with disproportionate fat distribution may experience higher mortality rates and increased complication severity. Notably, the waist-to-hip ratio can be a reliable indicator of health risks, surpassing the overall body mass index. This indicates that healthcare providers should use various measurements rather than solely rely on BMI. Moreover, research suggests that body composition can influence the effectiveness of certain treatments. For example, patients undergoing chemotherapy may have varying responses based on their metabolic status, often influenced by body fat percentage and muscle mass. The reliance on these metrics can guide personalized medicine approaches, ensuring that treatments are effectively aligned with individual risks based on body composition. Overall, understanding fat distribution enhances a clinician’s ability to interpret data associated with chronic diseases, allowing for customized treatment strategies aimed at improving outcomes.
Several chronic conditions intertwine with the complexities of body composition. Conditions such as obesity and metabolic syndrome pose significant health risks. They often lead to type 2 diabetes, hypertension, and cardiovascular diseases. Research highlights that individuals with greater muscle mass generally experience better health outcomes. Muscle plays a vital role in glucose metabolism, meaning patients with preserved or increased skeletal muscle may have lower insulin resistance. Hence, evaluating body composition gives insights into these interconnections. Regular assessments can help clinicians manage chronic diseases more effectively. For all patients, dietary interventions that promote healthy weight and muscle preservation are essential. Nutritional strategies might include increased protein intake, resistance training, and reducing simple carbohydrates. These changes can improve overall body composition. Additionally, educating patients on the importance of body fat distribution and muscle mass is vital for long-term health. Multidisciplinary approaches involving dietitians, physical therapists, and healthcare providers are often most effective. Using these insights, a healthcare team can create tailored programs aimed at improving body composition and, consequently, chronic disease prognosis.
Impacts of Aging on Body Composition
Aging significantly impacts body composition, particularly concerning muscle and fat distribution. As individuals age, they tend to lose muscle mass, a condition known as sarcopenia. The loss of muscle adversely affects mobility, increases vulnerability to falls, and poses additional health risks. Simultaneously, there can be an accumulation of visceral fat, compounding age-related health challenges. Comprehensive evaluations of body composition in older adults allow health professionals to establish baselines and monitor changes. Strategies to counteract these aging effects are crucial for maintaining health. Engaging in regular physical activity, especially resistance training, can help preserve muscle mass while reducing fat. Nutritional interventions focusing on higher protein intake can also be beneficial. Moreover, understanding the implications of aging on body composition serves as a prompt for preventative healthcare measures. Regular screenings can ensure that individuals remain vigilant about changes in their bodies, promoting timely interventions. Ultimately, addressing body composition in older patients contributes to an improved quality of life and better management of age-related chronic conditions.
The relationship between body composition and chronic disease outcomes emphasizes the role of lifestyle factors. Physical activity, nutrition, and mental health interrelate with body composition. Increased levels of exercise can enhance muscle mass while decreasing fat levels, improving overall health status and reducing chronic disease risks. Similarly, proper nutritional balance plays a pivotal role. Diets rich in lean proteins, whole grains, and healthy fats can contribute to favorable body composition. Moreover, addressing psychosocial factors is crucial, as stress and mental health can impact eating behaviors and lifestyle choices. Mental well-being intersects with physical health, influencing how individuals respond to treatment and adhere to preventive measures. Healthcare providers should take an integrative approach when considering body composition, incorporating discussions on lifestyle factors and mental health support. Patient education about the importance of an active lifestyle and balanced nutrition can empower them to make informed decisions. Patients equipped with knowledge regarding body composition, healthy habits, and disease risks can improve their engagement in healthcare and health management. As a result, patients may experience more favorable outcomes and overall improved health.
Future Directions in Body Composition Research
Research on body composition and its prognostic values in chronic diseases is evolving. The emergence of new technologies, such as advanced imaging techniques and artificial intelligence applications, promise to enhance our understanding of body composition dynamics. These innovations can enable more sophisticated analysis and better identification of at-risk populations. Future studies should focus on longitudinal assessments, which evaluate how body composition changes over time in chronic disease contexts. Investigating these changes will allow for earlier interventions and improved management strategies tailored to individual patient profiles. Moreover, interdisciplinary research combining insights from nutrition, exercise science, and behavioral health will deepen our understanding of how body composition influences chronic disease progress. Potential collaborations among healthcare professionals, researchers, and technologists can drive innovation, improving both research outcomes and patient care. Continuous funding and support for this avenue will be crucial for driving meaningful advancements. Furthermore, incorporating patient feedback in research designs ensures studies address real-world issues. Through this collaborative effort, the healthcare community can foster involvement in studies, enhancing overall health management for chronic disease populations.
In conclusion, the significance of body composition in chronic disease outcomes cannot be overstated. Its prognostic value is evident through the correlation between body metrics and disease progression. The potential for tailored treatment plans based on body composition assessments may improve patient care. By focusing on factors such as fat distribution and muscle mass, healthcare professionals can develop individualized programs to enhance overall health outcomes. The integration of lifestyle interventions presents opportunities for effective disease management. Future research and innovative technologies will pave the way for deeper insights into body composition’s role in chronic disease management. The healthcare community must remain committed to exploring these avenues and integrating findings into clinical practice. Ultimately, understanding the correlation between body composition and chronic diseases equips medical professionals with the knowledge necessary to improve patient outcomes. Patient-centered strategies should also motivate individuals to prioritize healthy living habits. By addressing body composition proactively, we can enhance quality of life for those at risk of chronic diseases, fostering a healthier future for all.