The Impact of Multiple Sclerosis on Coordination Abilities
Multiple sclerosis (MS) is a chronic neurological disease that affects the central nervous system. One of the most significant impacts of MS is on coordination abilities. Individuals with MS often struggle with balance and performing coordinated movements due to the demyelination of nerve fibers, which disrupts communication between the brain and muscles. This condition leads to various physical manifestations, making everyday tasks challenging. Coordination relies heavily on the brain’s ability to send signals smoothly to the body. In MS, these signals can be faulty or delayed, causing clumsiness or incoordination. The extent to which coordination is affected varies among individuals, depending on the severity of the condition and the specific areas of the nervous system that are most affected. This symptom profoundly impacts quality of life, limiting physical activity and increasing the risk of falls. Seeking assistance from healthcare professionals for tailored interventions improves the situation for many individuals. Understanding these coordination challenges is vital for developing effective treatment strategies. A multidisciplinary approach involving physical therapy and occupational therapy can help enhance mobility and confidence in those afflicted with MS.
Neurological Factors Affecting Coordination
Neurological factors play a critical role in the coordination issues associated with multiple sclerosis. The brain regions primarily responsible for coordination include the cerebellum and the basal ganglia. In patients with MS, lesions in these areas hinder optimal functioning, resulting in decreased balance, coordination, and fine motor skills. These impairments stem from the disrupted pathways that transmit sensory information and motor commands. Moreover, deterioration in muscle strength further complicates coordination challenges. Muscle weakness and spasticity can occur, adversely affecting gait and the ability to perform tasks smoothly. Additionally, the role of fatigue cannot be overlooked. Fatigue is a common symptom in MS patients, leading to decreased concentration and motivation to maintain coordination. Cognitive dysfunction also poses challenges, as attention deficits may cause missed steps in complex movements. Understanding these layered neurological factors highlights the complexity of MS’s impact on coordination abilities. Researchers continuously seek to gain insights into these mechanisms, striving to develop innovative therapies that enhance coordination. Improved understanding lends hope for tailored rehabilitation strategies that can improve the quality of life for individuals living with MS.
Coordination is not merely a physical ability; it requires cognitive engagement as well. MS can influence cognitive processes, further complicating coordination abilities. Cognitive impairment in MS may manifest as difficulties with attention, memory, and information processing speed. These cognitive challenges can diminish the effectiveness of motor planning, a crucial element in executing coordinated movements. As a result, individuals may find it challenging to initiate actions or respond promptly in situations requiring balance and precise movements. For instance, during simple tasks like walking on uneven surfaces or carrying objects, cognitive load can increase significantly. When cognitive functions decline, the brain struggles to coordinate sensory input with motor output. This disconnect can lead to increased fall risk and injuries, severely impacting independence. Engaging in cognitive training interventions can lend support, fostering enhancements in both cognitive and motor functions. Combining cognitive and motor training may offer a promising pathway for rehabilitation in MS patients. Therefore, a holistic approach targeting both physical and cognitive dimensions of coordination is crucial for improving overall function and promoting better health outcomes in individuals affected by MS.
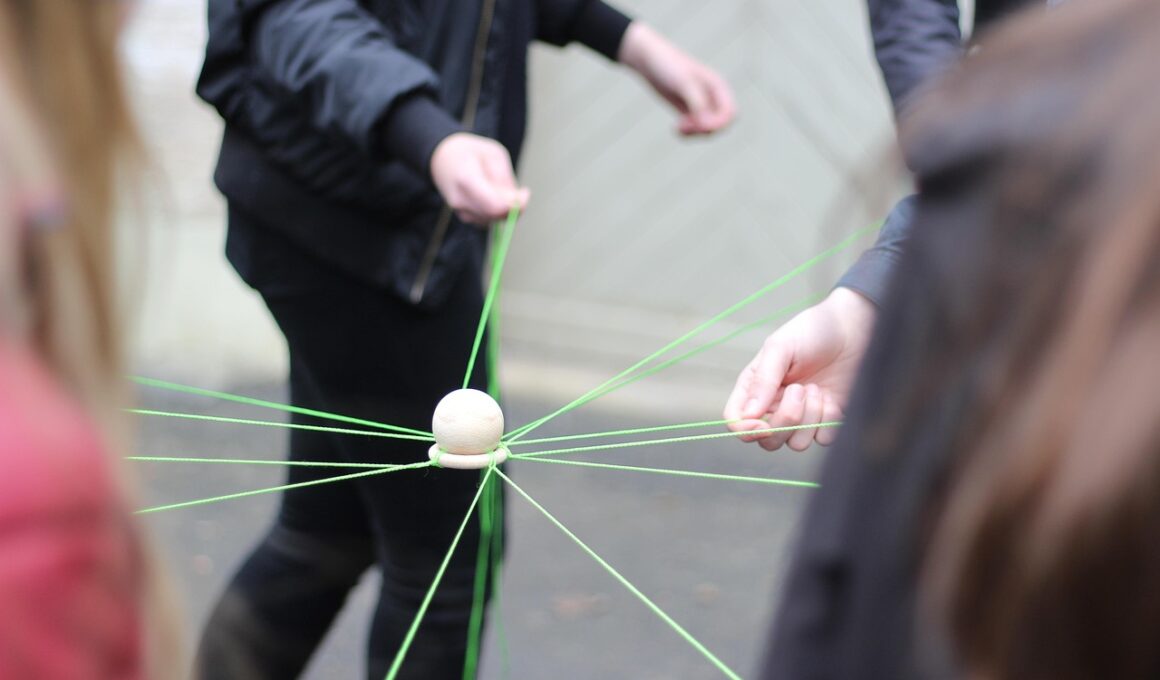
Physical rehabilitation plays a vital role in addressing coordination issues related to multiple sclerosis. Engaging in a structured physical therapy program helps strengthen muscles, improve balance, and enhance coordination abilities. These programs typically include flexibility exercises, gait training, and strength training tailored to individual capabilities, allowing patients to regain a sense of control over their movements. Moreover, balance training is vital in helping individuals enhance their stability during daily activities. Techniques such as proprioceptive training help individuals improve their awareness of body position in space. Occupational therapy complements physical therapy by focusing on daily living activities and adapting techniques or assistive devices to facilitate independence. Group therapy environments also foster motivation and social interaction, essential for emotional well-being. Incorporating regular exercise has shown to mitigate the physical and cognitive decline associated with MS. Patients who participate in consistent physical activity experience significant improvements in coordination and overall quality of life. Continued research into emerging therapies, including technology-based interventions, promises future advancements in rehabilitation approaches tailored to the unique coordination challenges faced by those living with MS.
Medications are often a necessary component of managing multiple sclerosis and its coordination disabilities. Disease-modifying therapies aim to reduce the frequency and severity of relapses but may also indirectly impact coordination. Some medications help manage specific symptoms, including spasticity and fatigue, which can further improve coordination indirectly. Individual responses to medications vary significantly, requiring careful monitoring and adjustment. It is essential for patients to work closely with healthcare providers to determine the most effective treatment plan. Additionally, addressing secondary conditions, such as pain, anxiety, and depression, may improve overall functioning and coordination. Psychosocial support has proven beneficial for individuals with MS, as mental health significantly impacts motivation and physical engagement. Counseling, support groups, and neuromuscular training interventions provide holistic support beyond medication alone. Employing a multi-faceted approach that combines pharmacological and non-pharmacological therapies enhances the ability to cope with coordination challenges stemming from MS. By focusing on personalized treatment strategies, healthcare providers can better equip patients with the tools necessary to navigate the complexities of life with multiple sclerosis.
Assistive devices can significantly aid individuals with multiple sclerosis in managing coordination disabilities. These devices range from mobility aids like canes and walkers to adaptive tools for performing daily tasks. They promote independence and confidence when moving through various environments, which is essential for mental well-being. Specific assistive technologies may also be beneficial; for instance, adaptive computer equipment helps individuals maintain skills in communication or work settings. Occupational therapists often assess patient needs and recommend appropriate assistive devices. Additionally, balance-enhancing footwear and orthotic devices can improve gait stability, reducing the likelihood of falls. Educating patients on the various tools available empowers them to make informed choices regarding their mobility and independence. With technology advancements, innovative solutions continually emerge, enhancing the quality of life for those affected by MS. The efficacy of these devices often depends on individual circumstances, making personalized assessments crucial. Incorporating these tools within the broader rehabilitation plan, including therapeutic exercises and education, forms a comprehensive strategy focusing on enhancing coordination abilities.
Family involvement and support are crucial for individuals coping with the coordination challenges associated with multiple sclerosis. Engaging family members in the rehabilitation process fosters a supportive environment, making it easier for patients to navigate daily life. They can provide physical support during therapies, assist with daily tasks, and encourage mobility activities. Moreover, understanding the challenges faced by their loved one promotes empathy and emotional connection, allowing families to offer better encouragement and reinforce motivation for rehabilitation. Educational resources for families about MS help them comprehend the condition and learn effective ways to support their relatives. Participating in support groups together can also create a shared understanding and strengthen familial bonds. Encouragement of independence, alongside necessary support, is pivotal in boosting self-esteem and enhancing coordination capabilities. Overall, a collaborative approach involving family members plays a vital role in reinforcing therapeutic goals and improving the prospects for individuals living with MS. By nurturing an environment filled with understanding and practical support, families become an integral part of aiding individuals in managing their coordination challenges effectively.
Ultimately, understanding the multifaceted nature of coordination challenges arising from multiple sclerosis empowers patients and healthcare providers alike. Acknowledging the interplay of neurological, cognitive, and physical factors enables a more comprehensive approach to treatment. Regular monitoring of symptoms and progress enhances rehabilitation strategies while informing patients about potential adjustments in their management plan. Continuous research into innovative therapies provides hope for those affected by MS, particularly concerning improving coordination functions. As understanding and awareness grow, advocating for coordinated treatment plans that address psychosocial elements alongside physical rehabilitation becomes increasingly necessary. Patients are encouraged to take an active role in their recovery, voicing their needs and collaborating with healthcare teams. Empowering patients in this way not only enhances their quality of life but also fosters resilience in the face of challenges. Collective efforts, including support from family and social networks, further bolster this process. With adequate resources and support, individuals with multiple sclerosis can find pathways toward increased functional independence and improved coordination abilities. This holistic approach will ideally lead to better outcomes, enabling individuals to thrive regardless of their diagnosis.