The Link Between Intermittent Fasting and Gut Motility
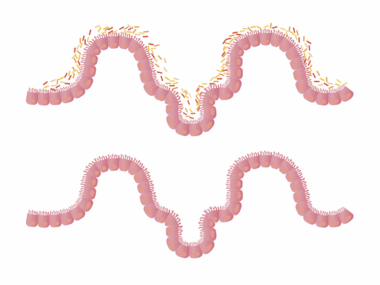
Intermittent fasting (IF) has gained significant attention for its potential health benefits, including its effects on gut health. One major aspect that researchers are examining is how IF influences gut motility. Gut motility refers to the contractions of the muscles in the gastrointestinal (GI) tract, which plays a crucial role in digestion and the movement of food through the intestines. Studies indicate that the timing of food intake during intermittent fasting may alter gut motility patterns. Changes in gut motility can impact nutrient absorption, and the overall health of the microbiome. Certain studies suggest that the cycling between feeding and fasting periods can help regulate hormones linked with digestion. When the gut has scheduled breaks from food intake during fasting, it may reduce the overall stress on the digestive system and optimize the function of gut bacteria. Understanding these dynamics can pave the way for future interventions that utilize fasting as a strategy to manage gastrointestinal health. In light of these findings, many individuals are exploring IF as a potential method to enhance gut health, further warranting detailed research in this field.
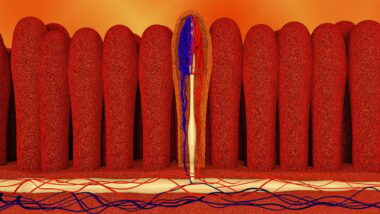
During intermittent fasting, different physiological changes occur, impacting gut health positively. For example, during fasting periods, the digestive system can undergo a process called autophagy, where old and damaged cells are removed and replaced. This process is crucial for maintaining a healthy gut lining, which can directly affect how well nutrients are absorbed. Enhanced absorption means that the body can efficiently utilize the vitamins and minerals available from food consumed during eating windows. Furthermore, research finds that a healthier gut lining may prevent issues like leaky gut syndrome, which can lead to inflammation and various gastrointestinal disorders. Prioritizing a healthy gut can enhance overall wellbeing, as a balanced gut results in better immune function and mental health. Incorporating intermittent fasting may also reduce symptoms of bloating, indigestion, and discomfort related to overeating. This methodology not only fosters a connection between feeding and fasting strategies with gut health but also encourages holistic health practices among followers of IF. As such, individuals considering this dietary approach should pay attention to their body’s signals to understand their unique responses to fasting.
The Role of the Microbiome in Gut Health
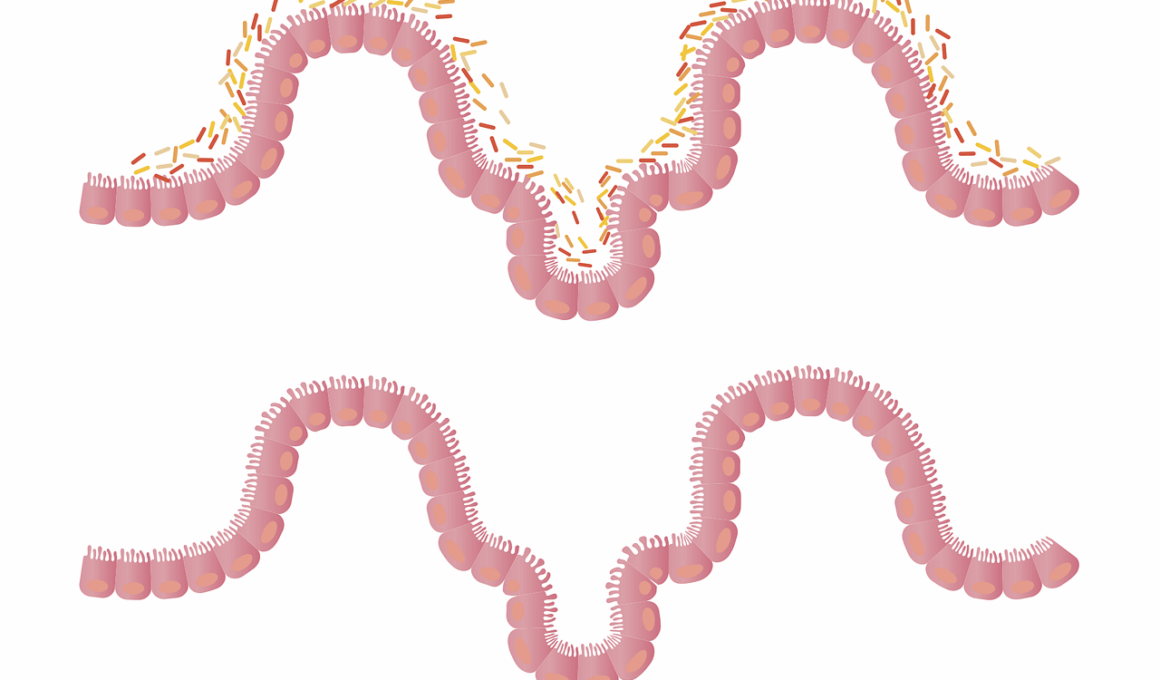
As research evolves, the importance of the gut microbiome continues to emerge, especially in the context of intermittent fasting. The gut microbiome comprises trillions of microorganisms that are crucial for digestion, metabolism, and immune system function. Evidence suggests that intermittent fasting can positively influence the composition and diversity of gut microbiota. A diverse microbiome is generally linked to improved digestive health and lower risk of chronic diseases. By limiting the time frame during which food is consumed, intermittent fasting may create favorable conditions for beneficial bacteria to thrive. Some studies indicate that fasting can increase populations of beneficial bacteria such as Lactobacillus and Bifidobacterium, known for their roles in enhancing digestion and reducing inflammation. Moreover, when the microbiome is balanced, the production of short-chain fatty acids, which are essential for gut health, is optimized. These fatty acids support gut barrier function and provide energy for colon cells. This multifactorial relationship between intermittent fasting and gut microbiota underscores the relevance of dietary patterns in influencing gut health. Meticulous attention to gut-friendly practices during fasting phases can aid in creating a resilient microbial population.
One interesting aspect of intermittent fasting is its potential impact on hormonal balance, particularly hormones that regulate appetite and digestion. For instance, during fasting periods, levels of growth hormone may increase, which can enhance fat metabolism and muscle preservation. Additionally, fasting can help in the regulation of insulin, which is essential for maintaining blood sugar levels. Improved insulin sensitivity can lead to better digestive outcomes, as stable blood sugar levels prevent energy dips that could affect gut functions. Similarly, fasting influences hormones such as ghrelin and leptin, which are crucial for appetite management. Proper regulation of these hormones can help avoid the binge-eating tendencies that may disrupt gut motility. When consumptions are controlled and done mindfully, it can foster better satiety signals, allowing individuals to make healthier food choices during their eating windows. Thus, understanding the hormonal responses elicited by intermittent fasting is paramount in harnessing its benefits for gut health. Furthermore, individuals practicing IF should aim to create a supportive eating environment to optimize their fasting experiences for maximum health enhancement.
Potential Risks and Considerations
While intermittent fasting holds promise for gut health, there are potential risks and considerations for those engaging in this dietary practice. One critical factor to keep in mind is individual variability in adapting to fasting protocols. People with pre-existing gastrointestinal disorders should consult healthcare providers before starting any fasting regimen. Individuals may experience digestive discomfort, bloating, or constipation if their fasting approach does not align with their unique digestive needs. Adequate hydration during fasting intervals becomes essential, as dehydration can exacerbate digestive issues. In particular, studies show that consuming sufficient fiber during eating periods can prevent constipation and support gut motility. Furthermore, the quality of food choices made during eating windows can affect overall gut health; high-sugar or processed foods may undermine the benefits of fasting. Thus, the integration of whole foods, probiotics, and prebiotics becomes pivotal in enhancing the benefits of intermittent fasting. Balancing the fasting approach with attention to dietary choices is vital for boosting gut health while reaping the rewards that intermittent fasting has to offer. Prioritizing education and self-awareness can aid individuals in navigating their fasting journeys safely.
Research continues to explore the mechanisms by which intermittent fasting can promote gut health, opening avenues for future study. Current investigations are focusing on the long-term impacts of intermittent fasting on gut microbiota composition and gut-associated disorders. One area of interest is how variations in fasting schedules can lead to different outcomes in digestive health. Furthermore, understanding the mechanisms underlying fasting-induced improvements in gut health can help in developing tailored dietary recommendations. As functional foods rich in prebiotics and probiotics gain popularity, the synergy between these foods and intermittent fasting might offer enhanced digestive benefits. Emerging research also seeks to clarify how intermittent fasting interacts with factors such as stress, sleep, and physical activity, all of which influence gut health. Scientists are emphasizing the importance of multi-disciplinary approaches to gain comprehensive insights into how fasting behaviors affect digestion, metabolism, and immune functioning. Increased public interest in gut health is prompting the need for more studies in diverse populations. Findings from such research can significantly contribute to public health initiatives and improve dietary guidelines in relation to intermittent fasting and gut motility.
Conclusion on Intermittent Fasting and Gut Health
In conclusion, intermittent fasting can offer potential benefits for gut health and motility, making it an intriguing dietary pattern for many individuals. With its influence on hormonal regulation and the microbiome, IF serves as a multifaceted approach to enhancing digestive wellbeing. However, one must consider individual differences, potential risks, and the importance of making mindful food choices during eating windows. As research continues to advance in the area of gut health, incorporating insights from scientific evidence can empower individuals to adopt sustainable dietary practices. Continued awareness of the relationship between fasting and gut health is essential for optimal health outcomes. Individuals are encouraged to approach intermittent fasting with curiosity and to pay attention to how their bodies respond. Engaging in this dietary practice could lead to significant improvements in digestive health and overall wellness. As society progresses in understanding the complexities of gut health, professionals and individuals alike should work together to harness the benefits of dietary approaches effectively. In summary, intermittent fasting represents a powerful tool to assist in fostering a thriving gut environment and improving overall health.
By paying close attention to the relationship between intermittent fasting, gut health, and overall wellbeing, individuals can take proactive approaches toward nourishing their bodies efficiently. For many, intermittent fasting serves as a means of not just weight management but also enhancing gut microbiota balance, contributing to physical and emotional health alike. Ultimately, embracing such dietary patterns requires education, individual adaptation, and community support to yield the most beneficial outcomes. The journey toward improved gut health through intermittent fasting can be a rewarding and empowering experience when approached thoughtfully. Further research will likely unveil new insights into the long-term impacts of intermittent fasting on gut health and digestion, helping to refine our understanding of nutrition and the microbiome. With time, practical applications can emerge to help every individual to optimize their unique relationships with food and fasting. This evolving body of evidence serves as an encouraging backdrop for anyone interested in maximizing their health through intentional eating habits. Thus, as more people look to intermittent fasting as a means of achieving vitality, the potential to shape healthier communities and lifestyles remains profound and promising.