The Role of Hormones in Vaccination Effectiveness
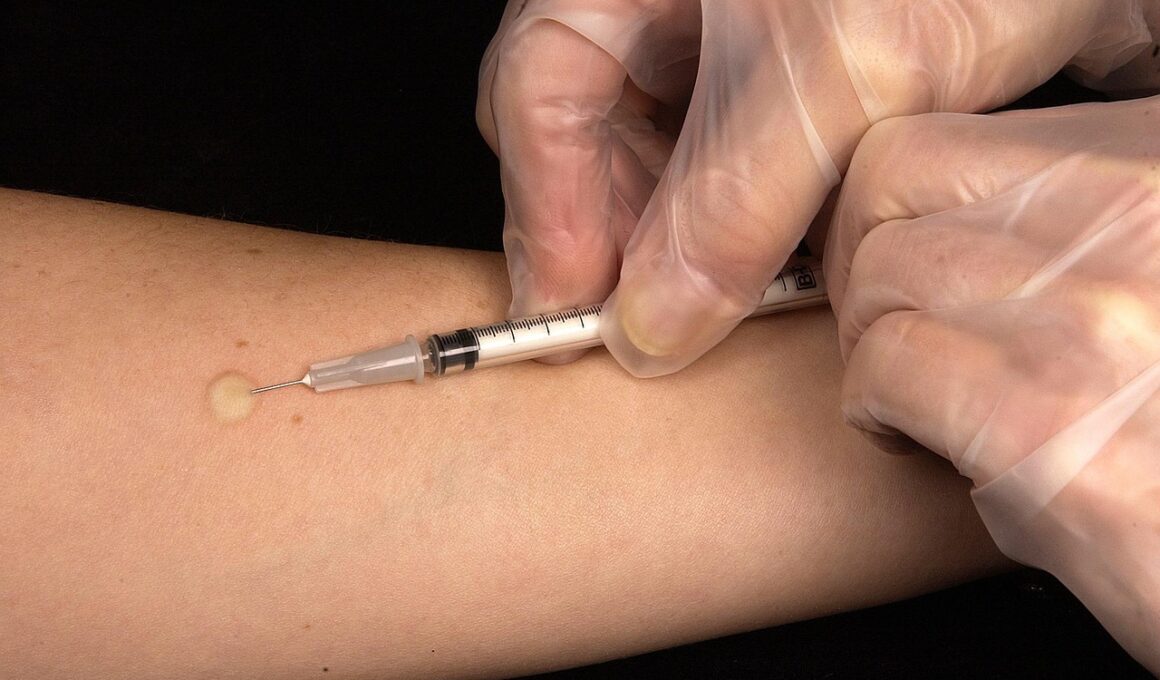
Vaccination is a cornerstone of public health that relies on the body’s immune response, influenced significantly by hormones. Hormones like cortisol, estrogen, and testosterone play crucial roles in modulating this immune response. Understanding how these hormones interact during vaccination provides insight into why some individuals respond better than others. Cortisol, often released in stress, can dampen immune reactions, while estrogen promotes immunity in females. For example, women generally exhibit stronger responses to vaccines, attributed to higher estrogen levels. Research shows that testosterone may impair response rates in men, suggesting that hormonal balance is critical in understanding vaccination outcomes. Additionally, factors such as age, health status, and lifestyle choices further influence these hormonal levels, subsequently affecting vaccine efficacy. Thus, the interplay between hormones and the immune system can help shape vaccination strategies. Tailoring vaccine interventions to account for hormonal differences among populations may enhance effectiveness. Further investigation into hormonal impact during vaccinations is essential for optimizing individual responses and improving the overall effectiveness of vaccination campaigns in diverse demographics.
Vaccine formulations are designed to induce an immune response, and hormonal levels may significantly affect this process. Immune system functionality can shift due to hormonal fluctuations, potentially leading to varying responses to vaccination. Hormones can modulate cytokine production, which plays a significant role in the immune response. These changes may lead to disparities in the antibody levels achieved post-vaccination. Additionally, psychological stress can influence these hormonal levels, notably affecting cortisol, which may reduce the overall immune efficacy. Recognizing these physiological impacts could lead to refined vaccination timing and strategies tailored to individual hormonal profiles. Moreover, exploring these correlations could reveal essential pathways for enhancing vaccine responses, particularly in populations that display high variability. Further studies are crucial to elucidate the mechanisms through which hormones affect vaccine efficacy. By implementing strategies to manage hormonal imbalances before vaccination, healthcare providers might improve vaccination outcomes. As new vaccines are developed, understanding the role of hormonal health will become increasingly essential, especially in the context of global vaccination efforts against emerging infectious diseases.
Hormones in Immune Function
The immune system is inherently complex and is profoundly influenced by hormonal health. Hormones such as glucocorticoids, derived from the adrenal glands, typically serve to regulate stress responses while modulating inflammatory pathways. During vaccination, a balanced immune response is crucial, as this determines the success of the inoculation. Furthermore, both male and female hormones can lead to differential immune responses between genders. Women tend to have enhanced immune responses during infections and vaccinations, often attributed to the effects of estrogen. This hormonal environment can accelerate antibody production. Conversely, elevated levels of testosterone in males may lead to a slower immune response, which could negatively impact the effectiveness of vaccinations. This gender discrepancy highlights the need for gender-specific vaccine dosing or scheduling. Additionally, considering hormonal therapies during vaccination periods may also enhance outcomes, particularly for populations with known hormonal imbalances. As research progresses, integrating this understanding into public health strategies could lead to improved vaccination approaches and overall health outcomes, underscoring the vital influence of hormones on vaccination effectiveness.
Further examination reveals that the timing of hormone fluctuations, notably during menstrual cycles or menopause in women, can affect vaccine responsiveness. Studies have shown that women receiving vaccines during certain phases of their cycles can achieve greater antibody responses, suggesting hormonal modulation can enhance immune efficiency. For example, administering flu vaccines during the follicular phase of the menstrual cycle can lead to superior outcomes. In men, hormonal changes such as seasonal variations in testosterone levels may affect vaccination responses as well. These insights emphasize the importance of considering hormonal states when scheduling vaccinations for different populations. Recognizing the impact of female reproductive hormones can empower healthcare providers to enhance vaccine efficacy based on gender. On a broader scale, public health initiatives could incorporate educational campaigns about hormonal health and vaccination timing to optimize immune responses. Further research is needed to understand the complex interplay of these hormonal effects fully. By tailoring vaccination strategies to accommodate these variations, we may boost public health vaccination rates, thus supporting overall community immunity during flu seasons and pandemics.
Stress and Hormonal Balance
Chronic stress can disrupt hormonal balance, profoundly impacting the immune system and, consequently, vaccination responsiveness. High cortisol levels due to stress might inhibit T-cell function and antibody production, leading to a less effective immune response post-vaccination. Addressing stress management techniques becomes crucial in optimizing vaccine efficacy, particularly for populations under high stress. Implementing stress-reduction strategies such as mindfulness, therapy, and physical activity may alleviate cortisol’s adverse effects, potentially enhancing how individuals respond to vaccines. Additionally, lifestyle factors like nutrition can influence hormonal health and the immune system, suggesting a holistic approach to vaccination preparedness. Adequate nutrition supports immune function and hormonal balance, emphasizing the interconnectedness of physical wellness and vaccine effectiveness. Community health programs focusing on lifestyle modification could enhance vaccination outreach efforts, targeting stress management and overall health improvement. Further insights could lead to practical applications of hormonal assessments before vaccinations, developing a comprehensive approach to improve individual and community immunization outcomes. In conclusion, establishing a comprehensive understanding of stress and hormonal influences will be essential for enhancing public health initiatives related to vaccination and disease prevention.
Emerging research continues to uncover new dynamics between hormonal health and vaccination efficacy, providing a rich area for exploration. For instance, studies examining the role of thyroid hormones have shown that imbalances can lead to altered immune responses, potentially complicating vaccination health outcomes. Individuals with hypothyroidism may have weakened immune responses, while those with hyperthyroidism could face increased risks of autoimmune reactions post-vaccination. These findings suggest that routine screening for thyroid function may be beneficial prior to vaccinations, particularly for vulnerable populations. Understanding the relationship between these hormones and the immune system could pave the way for personalized medicine approaches in vaccinations, where tailored strategies consider individual hormonal profiles. For example, hormonal assessments could guide vaccine selection or timing, leading to improved effectiveness and safety outcomes. Overall, the intersection of hormonal health and vaccination initiatives represents an essential frontier in immunology. By embracing this knowledge, healthcare providers can significantly improve vaccination efficacy and contribute to a healthier population overall. As ongoing studies emerge, the integration of hormonal health awareness into vaccination protocols could reshape public health practices globally.
Future Directions
As the science surrounding hormones and the immune system continues to evolve, new avenues of research will provide deeper insights into vaccination effectiveness. Future studies may explore genetic factors that influence hormonal responses to vaccines, further elucidating the role of personal biology in immunization outcomes. By integrating immunology, endocrinology, and genetics, researchers can develop a comprehensive model of vaccination responses. Public health policy must adapt to incorporate these findings, ensuring that vaccination campaigns become more effectively tailored to individual needs based on hormonal health. For instance, genetic screenings might identify individuals who could benefit from adjusted vaccine dosage or alternative formulations, paving the way for advanced immunization practices. Collaborative efforts across different scientific domains will be essential in adopting these advancements in clinical practice. Ultimately, the goal remains clear: improving vaccination effectiveness through a robust understanding of hormones. Attention to this interplay provides an opportunity for personalized healthcare approaches, enabling better public health outcomes. The synergy of hormone and immune system studies will undoubtedly foster innovation in vaccine development, significantly impacting global health strategies and preventive medicine.
In summary, the interface between hormones and vaccination effectiveness represents a growing field of research with significant implications. Understanding how hormonal levels affect immune responses can lead to more effective vaccination strategies, particularly for diverse population groups. By analyzing the interplay of stress, hormonal health, and immune function, public health approaches can become more tailored and impactful. Future research initiatives must focus on unraveling these complex interactions and translating findings into clinical practice. Enhanced education for health professionals about hormonal influences on immunization should also be prioritized, ensuring that vaccination campaigns are optimized. With the right focus and resources directed towards the study of hormones, the aim of achieving higher vaccination rates and improved public health can be realized. The relationship between these biological factors and immunization can reshape not only public health strategies but also individual health outcomes. Hormonal health awareness can significantly influence vaccination campaigns, underscoring the importance of an integrated approach in public health. As research progresses, translating findings into actionable strategies will be essential for harnessing these insights to bolster vaccination efforts in communities worldwide.