Intermittent Fasting and Heart Disease: What You Need to Know
Intermittent fasting (IF) has gained attention for its potential health benefits, particularly regarding heart health. However, those with heart disease or other chronic conditions should approach IF with caution. It’s crucial to understand how fasting might interact with various medications and lifestyle choices. Consulting with healthcare providers is essential before making significant dietary changes. Heart disease patients must monitor their health closely during fasting periods, considering factors like blood pressure and cholesterol levels. In some cases, fasting can lead to harmful spikes or dips in these levels. Proper hydration is vital, as dehydration can adversely affect heart function. Be aware of symptoms that may arise from fasting, including dizziness or fatigue, and seek medical advice when needed. Individual responses to fasting can vary significantly, highlighting the importance of personalized strategies in dietary planning. In conclusion, while IF shows promise for better heart health in some individuals, patients with chronic conditions must prioritize safety by working with healthcare professionals. Making informed decisions based on professional guidance can help maximize benefits while minimizing risks associated with intermittent fasting.
Fasting can influence hormones, particularly insulin and cortisol, which play vital roles in metabolic health. Both heart disease and diabetes require careful management of these hormones for optimal health outcomes. Intermittent fasting may improve insulin sensitivity for some, which is crucial for heart disease patients with insulin resistance. Additionally, fasting can reduce inflammation, which is a contributing factor to heart disease progression. However, patients must recognize that these benefits are not guaranteed and largely depend on individual circumstances. For those taking certain medications, timing their intake around fasting can prevent potential complications. It’s essential to listen to your body during these fasting windows. If heart disease patients experience any adverse effects, it may be wise to adjust fasting protocols or discontinue them altogether. Having a structured plan with flexibility to adapt based on bodily responses can help. Moreover, education is key—understanding how different types of fasting might affect individual health conditions is crucial for success. Research continues to evolve in this area, allowing better understanding and guidelines to emerge for patients. Remaining informed will empower individuals with heart disease to make the best choices.
Precautions for Chronic Illnesses
When considering intermittent fasting for heart disease, there are several precautions to keep in mind to ensure safety. For instance, individuals should prioritize balanced nutrition during eating windows. Nutrient-dense foods provide essential vitamins and minerals that support cardiovascular health. Food choices can significantly impact fasting outcomes, especially in maintaining stable blood sugar levels. Including high-fiber foods can be beneficial, aiding digestion and promoting a sense of fullness. Additionally, it’s essential to maintain regular monitoring of heart-related symptoms during fasting periods. This proactive approach can help identify potential issues early. Collaboration with a dietician can assist in crafting meal plans that align with fasting schedules while addressing nutritional needs. Disregarding these precautions may lead to adverse effects, undermining any potential benefits of fasting. Patients should also educate themselves about the potential side effects of fasting, such as sudden drops in energy levels or emotional changes. Communication with healthcare providers about experiences during fasting is vital. By being informed and vigilant, heart disease patients can successfully navigate the landscape of intermittent fasting.
Furthermore, considering the psychological impacts of intermittent fasting is crucial for those with chronic illnesses like heart disease. Changes in dietary patterns and eating behaviors can induce stress or anxiety in vulnerable individuals. Establishing a supportive social network can help maintain motivation and adherence to fasting routines. Engaging friends or family in discussions around fasting may relieve stress and foster a positive environment. Mindfulness practices, such as meditation or yoga, can also enhance coping mechanisms related to dietary changes. It’s important to recognize that intermittent fasting isn’t suitable for everyone. Some individuals may experience elevated stress levels, while others may thrive on a structured eating schedule. Tailoring fasting approaches to fit personal comfort levels and lifestyles can promote long-term success. In addition, daily routines can also play a role in fasting experiences. Prioritizing adequate sleep helps the body recover and adapt to fasting periods. Maintaining a consistent sleep pattern supports metabolic health, which is crucial for heart disease management. By combining mindful practices with dietary strategies, heart disease patients can ensure healthier outcomes.
Potential Benefits of Intermittent Fasting
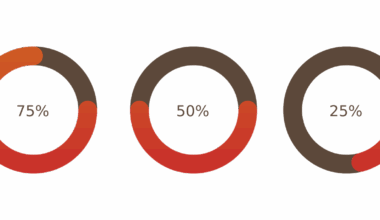
Many studies suggest that intermittent fasting can offer potential benefits, particularly in cardiovascular health. These benefits revolve around weight management, where fasting can aid in reducing body fat and visceral fat accumulation. By minimizing excess weight, individuals lower their risk of heart disease and related complications. Moreover, fasting may also help improve cholesterol levels. Lowering LDL cholesterol and triglycerides while increasing HDL cholesterol can potentially enhance heart health. Additionally, intermittent fasting has been associated with improved blood pressure regulation, which is essential for heart disease patients. Enhanced metabolism is another fascinating aspect of fasting; it can stimulate the body’s natural mechanisms for repairing and regenerating cells. Studies highlight the activation of autophagy, a process where cells remove damaged components, promoting overall better health. However, while these benefits sound promising, individual responses can greatly vary, emphasizing personalized approaches. Those with chronic illnesses, including heart disease, should be cautious and avoid universal application of fasting strategies. Monitoring health indicators through regular check-ups can help track improvements or challenges brought by fasting.
Incorporating intermittent fasting into daily life may require some adjustment for heart disease patients. Creating a manageable fasting schedule is vital for ease of implementation. Choosing a feasible eating window while accommodating individuals’ work and social obligations can enhance adherence. Notably, flexibility can help simplify dietary changes. Maintaining variety in meals prepared during eating windows can make the experience enjoyable and less tedious. Exploring new recipes and cooking styles keeps individuals engaged and motivated. Educating oneself on the types of fasting—like alternate-day fasting or the 16/8 method—can help in selecting the most suitable option. Furthermore, it’s important to stay informed regarding research updates about fasting’s effectiveness and safety in heart disease management. Participating in communities or forums dedicated to fasting can provide support and encouragement. Sharing experiences, tips, and progress may positively influence motivation and sustainability. A well-rounded approach that encompasses fasting, nutrition, and fitness can offer the greatest long-term benefits. Remember, every journey is unique, and finding what works best for individuals can enhance overall quality of life while managing heart disease.
Conclusion and Key Takeaways
In summary, intermittent fasting can provide potential benefits for individuals with heart disease but requires a cautious approach. Consulting with healthcare professionals is essential to ascertain its suitability based on individual health conditions. Tailoring fasting methods and maintaining a focus on nutrient-dense foods can optimize results. Individuals should prioritize hydration and listen to their bodies during fasting periods. Monitoring health indicators and symptoms can help in evaluating the effects of fasting. Building a support network can provide motivation and encouragement, easing the transition into a fasting routine. Mindfulness and stress management techniques can further enhance the experience, making dietary changes more manageable. Ultimately, fasting should not be one-size-fits-all; personalized approaches based on individual needs and responses ensure safety. Ongoing research continues to shed new light on the relationship between intermittent fasting and heart health. Staying informed will empower heart disease patients to make educated nutritional choices moving forward. Committing to a healthy lifestyle, including proper diet and exercise, remains critical in improving heart health. The key is defining a sustainable strategy that supports overall wellness.
As interest in intermittent fasting grows, we encourage individuals with chronic conditions to remain proactive in seeking education and peer support. The right resources can make all the difference in one’s health journey. Many online communities and resources now discuss fasting strategies tailored to chronic illnesses. Engaging in conversations about shared experiences can foster camaraderie, dispelling feelings of isolation. Additionally, utilizing nutrition apps can assist in tracking food intake and fasting schedules, allowing for more informed choices. Ultimately, the pursuit of heart health embraces a holistic view, integrating proper diet, physical activity, and mental wellness. By equipping themselves with knowledge and tools, individuals can navigate the world of intermittent fasting confidently. This approach will promote better heart health and longevity for those with chronic conditions. Education may empower individuals to take charge of their health, guiding them toward optimal choices. As everyone’s journey is unique, finding the perfect balance will enhance the quality of life and foster a brighter outlook on health. Seeking the advice of medical professionals and dieticians remains essential in this process to ensure safety and efficacy.