Fasting, Metabolism, and Hypertension: A Holistic View
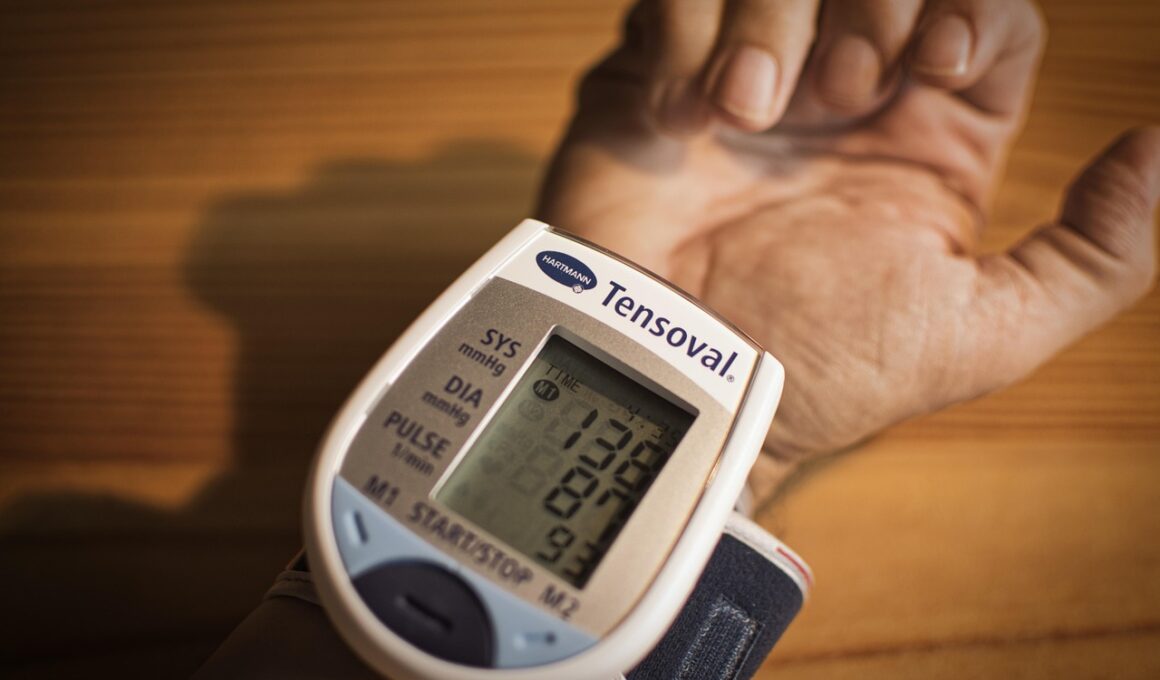
Intermittent fasting (IF) has gained popularity as a dietary method that not only aids in weight loss but also provides significant health benefits, particularly in relation to hypertension. Hypertension, or high blood pressure, is a chronic condition that can lead to severe health complications like heart disease and stroke. Recent studies suggest that engaging in intermittent fasting may play a crucial role in managing blood pressure levels. During fasting, the body enters a state of physiological stress which can trigger processes like autophagy and ketosis. These processes help cells rejuvenate and reduce inflammation. Furthermore, fasting may influence hormonal changes that optimize blood pressure regulation, such as improved insulin sensitivity. Moreover, certain protocols, like the 16/8 method or alternate-day fasting, are being examined for their effectiveness in lowering blood pressure. It’s essential to note that while fasting may offer solutions, it should be approached cautiously and ideally under medical supervision, especially for individuals already facing hypertension challenges. Regular monitoring of blood pressure during fasting can provide insights into its effects, ensuring that safety is prioritized while exploring this holistic dietary approach.
How Fasting Affects Blood Pressure
Numerous studies have explored how intermittent fasting directly influences blood pressure. The primary mechanism includes improved vascular function facilitated by weight loss, reduction in visceral fat, and hormonal adjustments. During fasting periods, several metabolic processes initiate that can improve endothelial function. For instance, levels of nitric oxide, a vasodilator, may increase, thereby helping to relax blood vessels. Additionally, intermittent fasting can decrease levels of cortisol, the stress hormone, which is known to contribute to hypertension when persistently elevated. It’s worth noting that hydration and nutrient intake during feeding windows are equally crucial. Proper hydration can help maintain optimal blood viscosity and blood flow, while a diet rich in potassium and magnesium can support healthy blood pressure. Recommendations increasingly emphasize consuming whole, nutrient-dense foods rather than processed options during eating periods to maximize cardiovascular benefits. Therefore, individuals interested in fasting as a strategy to improve hypertension should focus on not just fasting but also on holistic dietary practices that promote and maintain heart health. Combining fasting with balanced nutrition may yield optimal blood pressure control.
The influence of intermittent fasting on hypertension is not merely physiological; it also has psychological components worth exploring. Stress and anxiety are frequently linked to high blood pressure, and fasting could serve as a stress-management tool for some individuals. The discipline required in adhering to a fasting schedule can help instill a sense of control over one’s lifestyle choices. Additionally, many individuals report mental clarity and increased energy levels during fasting periods, which can positively contribute to managing stress. Mindfulness practices and meditation, often incorporated alongside fasting, can further enhance psychological well-being, combating factors that exacerbate hypertension. Moreover, the community aspect of intermittent fasting, where individuals share their experiences and support each other, brings a social component that can be beneficial for mental health. Engaging with supportive groups, either in-person or online, creates a sense of accountability and motivation that can reduce stress and anxiety. The interplay between fasting, mental clarity, and social support emphasizes the holistic nature of managing hypertension. Thus, the mental benefits of fasting should not be overlooked as part of a comprehensive strategy to alleviate high blood pressure.
Nutritional Considerations during Fasting
Nutritional choices during eating windows are pivotal for anyone practicing intermittent fasting, especially individuals with hypertension. The ideal diet should include foods rich in antioxidants, potassium, and omega-3 fatty acids to support cardiovascular health. Leafy greens, berries, nuts, and fatty fish are all beneficial options. These foods contribute not only to well-being during fasting but also help mitigate high blood pressure. Additionally, managing sodium intake is crucial; excessive sodium can cause fluid retention, leading to elevated blood pressure. Many processed foods contain hidden salts that can derail efforts to maintain healthy blood pressure levels. Intermittent fasting can encourage better food choices; with a defined eating window, there is often more focus on quality over quantity. Incorporating fibrous foods during feeding periods aids in digestion and contributes to metabolic health, diminishing the chance of blood pressure spikes. Further, timing meals appropriately can enhance nutrient absorption. To achieve desired results, individuals are encouraged to consult healthcare professionals or dietitians who can offer tailored advice on meal planning that aligns with both fasting and hypertension management.
While intermittent fasting offers potential health benefits, it is crucial to tackle the topic of safety and individual variability. Not everyone responds to fasting in the same way, and medical conditions can significantly influence outcomes. For individuals with high blood pressure, careful consideration must be given to their unique health profiles, comorbid conditions, and medications. For instance, those on antihypertensive medications need to monitor blood pressure regularly, as fasting may influence drug absorption or effectiveness. Additionally, if fasting results in significantly lower blood pressure, adjustments to medication dosages may be necessary. Furthermore, individuals with conditions like diabetes or eating disorders should approach intermittent fasting with increased caution and under professional guidance. The potential for adverse effects increases when fasting is adopted without proper knowledge or medical oversight. Therefore, engaging with healthcare providers to devise a fasting strategy tailored to individual health needs ensures a safer approach. Being well-informed about the possible effects and recognizing one’s body’s response are essential steps in safely experimenting with intermittent fasting as a means to manage blood pressure.
Clinical Evidence of Fasting Benefits
The growing body of clinical evidence supporting intermittent fasting indicates promising outcomes regarding hypertension reduction. Various studies have demonstrated significant drops in both systolic and diastolic blood pressure among participants who incorporate fasting regimens into their lifestyles. For instance, one study found that alternate-day fasting led to an average reduction in blood pressure markers among participants who adhered strictly to the protocol. Another study highlighted the importance of combining fasting with moderate exercise to amplify blood pressure regulation. Furthermore, systematic reviews have analyzed outcomes suggesting that these fasting methods may even be more beneficial than traditional calorie restriction when it comes to cardiovascular health. The importance of consistent monitoring of blood pressure before, during, and after fasting cannot be overstated, as it provides crucial insights into individual responses. As research advances, ongoing exploration into the mechanisms behind these benefits continues. This includes examining genetic factors that might influence individual responses to fasting. The emerging evidence bases encourages a receptive mindset towards adopting fasting as a viable strategy for managing hypertension, where personal experiences and clinical insights can guide future implementation.
In conclusion, intermittent fasting emerges as a multifaceted approach to managing hypertension and enhancing overall health and well-being. It combines physiological, psychological, and nutritional benefits that collectively support heart health and weight management. Elevated blood pressure is a significant health concern; thus, adopting practices that promote wellness, such as fasting, can be a transformative step towards a healthier lifestyle. It’s crucial, however, to approach fasting with a balanced view of its benefits and challenges. Individual health conditions and lifestyle preferences must align with any fasting regimen adopted. Ongoing research continues to illuminate the myriad effects of fasting on various health parameters, providing additional instructions for practice. Engaging with healthcare professionals remains vital to ensure that fasting aligns with medical advice and personal health priorities. Furthermore, social and community engagement can bolster commitment to fasting practices while offering emotional support. As attention towards holistic health strategies grows, intermittent fasting may serve as an essential tool in the management of hypertension, giving individuals a pathway to better health through informed choices.