Evaluating Fatigue in Chronic Illness by Assessing Muscle Mass
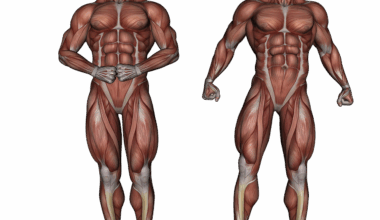
Chronic illnesses significantly impact the quality of life, often resulting in persistent fatigue. One key factor in understanding this fatigue is muscle mass, which plays a pivotal role in overall body composition. Evaluating body composition through muscle mass provides valuable insights into how chronic diseases affect physical health. Muscle mass is essential for strength, mobility, and overall energy expenditure. In individuals with chronic diseases such as diabetes, heart disease, and chronic obstructive pulmonary disease, decreased muscle mass can exacerbate feelings of fatigue. Furthermore, the loss of muscle mass may result from inflammation, metabolic changes, and reduced physical activity. Assessing muscle mass allows healthcare providers to tailor interventions to improve patient outcomes. It may involve a combination of nutritional support and exercise programs specifically designed to enhance muscle mass. Consequently, it is crucial to monitor muscle mass regularly in patients with chronic conditions. Utilizing techniques such as dual-energy X-ray absorptiometry (DXA) or bioelectrical impedance analysis (BIA) can provide accurate measurements. These techniques help identify muscle wasting and enable timely interventions that can mitigate fatigue and enhance the overall quality of life.
The Role of Muscle Mass in Chronic Diseases
Muscle mass and its preservation are critical in sustaining overall health, especially in individuals with chronic diseases. Maintaining muscle mass is linked to better functional capacity and reduced fatigue; thus, understanding its role is vital. Chronic conditions often hinder physical activity, which leads to muscle mass loss. For example, cancer patients frequently experience cachexia, a syndrome characterized by significant loss of body weight and muscle mass. This phenomenon can profoundly affect their strength and energy levels. Patients with chronic kidney disease also suffer from protein-energy wasting, making muscle preservation a significant concern. Additionally, in aging populations, sarcopenia—a condition involving age-related muscle loss—affects chronic disease management. Regular assessment of muscle mass should be prioritized by healthcare providers in these cases. Assessing muscle mass can guide nutritional interventions tailored to increase protein intake or exercise programs focused on resistance training. Interventions can help slow muscle loss, increase strength, and decrease fatigue. Understanding the connection between chronic diseases and muscle mass is essential for effective patient care and improving treatment strategies.
Fatigue is a multifaceted symptom experienced by individuals with chronic illnesses, and its connection to muscle mass cannot be overlooked. Chronic inflammation often affects the body’s response to exercise and can lead to decreased muscle health. Muscle atrophy, or the wasting of muscle tissue, can result from prolonged inactivity due to illness, enhancing feelings of fatigue. Evaluating muscle mass offers an objective measure to empower healthcare providers in understanding the fatigue experienced by their patients. Specific assessments, including strength testing and functional performance measures, can reveal correlations between muscle mass and energy levels. Moreover, proper interventions, like strength training and nutritional supplementation, can address these concerns effectively. It has been advocated that increasing muscle mass through targeted exercise regimens can combat fatigue. Additionally, educating patients about the importance of maintaining muscular health is necessary. The psychological impact of fatigue can also be mitigated through awareness of this relationship, motivating patients to engage in healthy behaviors. Thus, comprehensive evaluations in clinical settings can be beneficial in managing fatigue effectively. Close cooperation between patients and healthcare providers will foster better outcomes.
Interventions to Combat Muscle Loss
To counteract the effects of muscle loss and fatigue in chronic diseases, several interventions can be implemented. Firstly, nutritional support emphasizing high-protein diets can play a critical role in maintaining muscle mass. Incorporating high-quality protein sources such as lean meats, legumes, and dairy products into daily meals may promote muscle synthesis. Additionally, personalized exercise programs that focus on resistance training can be beneficial in restoring muscle mass. Such programs should be tailored to individual capabilities and can significantly boost strength and functionality. Studies indicate that, even in frail patients, appropriate exercise can improve muscle function and reduce fatigue levels. Furthermore, engaging patients in educating them about the importance of nutrition and physical activity can empower them to take control of their health. For patients with more severe complications, nutritional supplements specifically designed for muscle preservation may be considered. These specialized products can support dietary intake, ensuring that individuals receive adequate nutrients. Therefore, an integrative approach that incorporates dietary and exercise modifications is essential for effectively addressing fatigue in chronic illnesses related to muscle mass.
The psychological aspects of dealing with chronic illness-associated fatigue are significant but often understated. Individuals may experience feelings of helplessness, anxiety, and depression due to their fatigue and diminishing muscle strength. These emotional challenges can create a negative feedback loop, leading to further inactivity and muscle deterioration. Addressing these psychological factors is vital for fostering resilience in patients managing chronic illness. Healthcare providers must approach this complexity with appropriate resources, including mental health support and counseling. Encouraging social support networks can play a vital role in diminishing feelings of isolation patients may face. It’s also important to foster communication and encourage patient engagement in their treatment regimen. Behavioral therapies can equip individuals with skills to cope with fatigue and its underlying causes. Regular monitoring of symptoms and progress in muscle mass can help adjust intervention strategies accordingly. By taking a multi-dimensional approach to treat fatigue, patients are more likely to see improvements in both muscle mass and overall energy levels. Consequently, integrating mental health considerations into treatment plans is essential for a holistic approach in addressing chronic diseases.
Implementing Comprehensive Assessments
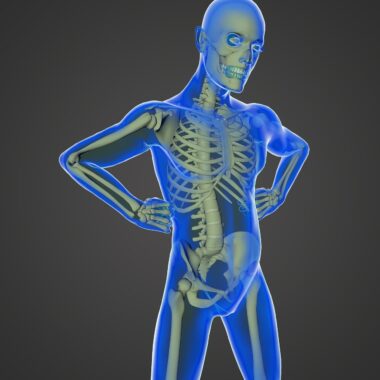
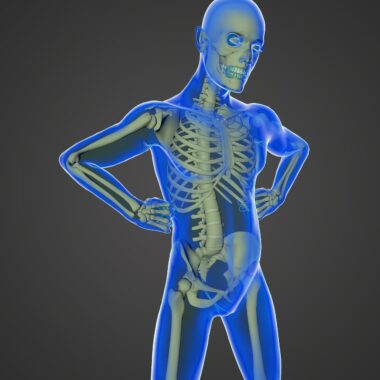
Implementing comprehensive assessments in clinical practice can reveal critical insights into the role of muscle mass in fatigue. Regular monitoring through advanced techniques provides healthcare professionals with pertinent data. Utilizing tools like dual-energy X-ray absorptiometry (DXA) grants an accurate depiction of body composition changes over time. Keeping up-to-date records of muscle mass can reveal patterns, guiding interventions for individual patients. Employing bioelectrical impedance analysis (BIA) offers another innovative approach to assess body composition and muscle mass. These methods not only measure but also inform on the effectiveness of therapeutic interventions. Efficient tracking can aid in determining if prescribed nutritional and exercise regimens are having the desired impact. Additionally, healthcare providers may find it advantageous to use subjective measures of fatigue in tandem with objective assessments of muscle mass. Insufficient energy levels can sometimes indicate underlying issues that require further investigation. Therefore, combining subjective and objective measures offers a more detailed assessment of the patient’s condition. Overall, comprehensive assessments must become integral components of care planning in patients experiencing fatigue due to chronic illnesses and muscle mass declines.
In conclusion, understanding muscle mass’s vital role in evaluating and managing fatigue in chronic diseases is essential. By recognizing the correlation between reduced muscle mass and increased fatigue, healthcare providers can develop targeted interventions. Focused nutritional strategies and personalized exercise programs foster muscle preservation and bolster patients’ energy levels. It is equally important to address psychological aspects surrounding fatigue; emotional support plays a significant role in coping with chronic disease challenges. Comprehensive assessments of muscle mass serve as critical tools in identifying and managing fatigue effectively. Enabling regular evaluations can lead to timely adjustments in patient care strategies. As research continues, advances in body composition analysis will further enhance understanding in this area. Integrating innovative assessment methods will lead to better patient outcomes, improved quality of life, and effective fatigue management. Collaborating with patients and addressing their individual needs will promote adherence to treatment strategies, leading to successful interventions. Ultimately, assessing and maintaining muscle mass in chronic diseases is paramount for improving functional capacity and managing symptoms of fatigue.