The Future of Intermittent Fasting Research in Inflammation Management
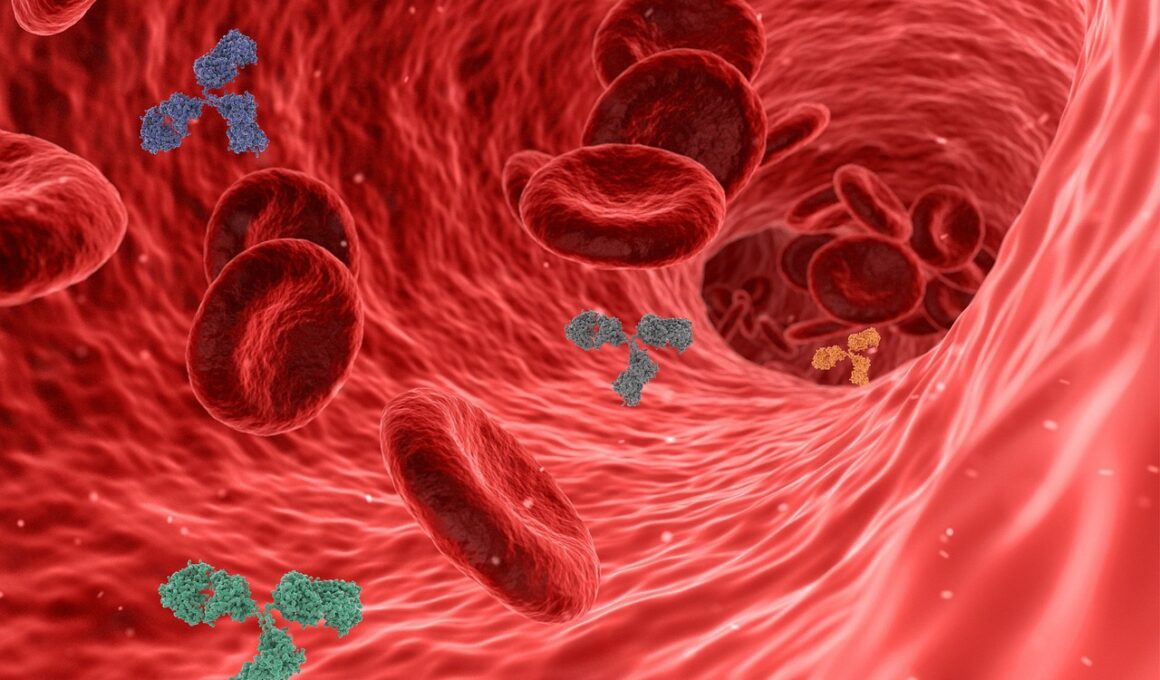
Intermittent fasting (IF) has become a popular dietary approach, increasingly studied for its myriad health benefits. Inflammation is a critical area of focus in health research, as it is linked to numerous chronic diseases. Emerging studies suggest that IF may play a role in modulating inflammatory processes. By periodically restricting caloric intake, IF may trigger biological responses that decrease inflammation markers in the body. This relationship is essential for understanding how dietary practices can influence health outcomes. Individuals experiencing conditions associated with chronic inflammation, such as arthritis or cardiovascular disease, could potentially benefit from adopting an intermittent fasting regimen. Nevertheless, further investigation is needed to establish the exact mechanisms through which IF affects inflammation. The idea is that metabolic changes during fasting might signal cells to employ protective mechanisms against inflammation. Additionally, researchers are keen to explore how the timing and duration of fasting contribute to these effects. Hence, the quest to uncover the intricacies of IF and inflammation continues to gather traction and promises fresh insights in health science.
Inflammation’s relationship with diet isn’t new, with various dietary approaches claiming effects in reducing inflammatory conditions. The role of IF in this landscape is particularly fascinating since it encompasses not just what we eat, but when we eat it. The evidence gathered thus far indicates that IF might reduce levels of harmful inflammatory markers such as C-reactive protein (CRP). CRP is often used as a biomarker to assess inflammation levels in the body. By reducing these markers, IF potentially lowers the risk of developing chronic illnesses attributed to inflammation. Some studies even show that IF can enhance the body’s resilience to stress, a significant factor in managing inflammation. Importantly, studies suggest that the benefits of IF are likely influenced by individual factors, including age, sex, and baseline health status. Understanding these variables is vital as it may determine how effectively IF can manage inflammation for different populations. Researchers aim to break down these differentiating factors to establish tailored fasting protocols that could enhance health outcomes across various demographics.
The Science Behind Intermittent Fasting and Inflammation
Recent research has illustrated that intermittent fasting, when practiced correctly, can lead to remarkable biological changes that promote better health. One notable shift during fasting periods is the alteration in the production of pro-inflammatory cytokines. These signaling molecules play a pivotal role in initiating and sustaining inflammatory responses. By restricting the window of food intake, IF can potentially recalibrate the body’s inflammatory response. Moreover, a fascinating aspect of IF is its potential to facilitate autophagy—a cellular cleanup process that targets damaged cells and proteins. This process may help the body to combat inflammation at a cellular level, thus mitigating chronic diseases. Additionally, the ability of IF to lower insulin levels further serves to reduce inflammatory responses, as elevated insulin is often associated with chronic inflammation. As such, ongoing studies are focused on whether certain types of fasting methods—like alternate-day fasting or time-restricted eating—are more effective in promoting anti-inflammatory effects. Unraveling the connections between fasting protocols and inflammation can potentially pave the way for novel dietary strategies in disease management.
Despite the promising findings surrounding intermittent fasting, challenges remain in the landscape of research evaluating its role in inflammation management. One significant barrier is the heterogeneity in study designs, which includes differences in participant characteristics, fasting protocols, and duration of studies. This variability can complicate the interpretation of results, making it difficult to draw definitive conclusions. Increased standardization in methodologies will enhance the comparability of findings and promote wider acceptance of IF as an anti-inflammatory intervention. Furthermore, long-term effects of intermittent fasting remain somewhat elusive, as most studies focus on shorter durations. Longitudinal investigations are critical to ascertain how sustained fasting impacts inflammation and overall health. Researchers are also examining potential adverse effects or challenges individuals may face when adopting fasting regimes. Psychological aspects, such as adherence and the potential for disordered eating patterns, also warrant attention. As the field evolves, understanding these multidimensional aspects will be necessary for developing guidelines that ensure safety and efficacy when implementing fasting strategies in daily life.
Practical Implications for Those Interested in Intermittent Fasting
For individuals considering intermittent fasting to manage inflammation, practical considerations should be taken into account. Firstly, it is essential to understand that intermittent fasting is not a one-size-fits-all approach. Consulting healthcare professionals before embarking on such dietary changes is advised, particularly for those with underlying health issues. Creating a fasting plan that aligns with personal lifestyle, preferences, and health goals is vital for achieving long-term success. Moreover, focusing on nutrient-rich foods during eating windows enhances the anti-inflammatory effects of fasting, as whole foods are packed with essential nutrients and antioxidants. Staying adequately hydrated and incorporating physical activity also contribute to improved health outcomes. Notably, listening to your body and being aware of its responses to fasting is crucial; if adverse effects occur, reconsideration of the fasting strategy may be necessary. Keeping a journal to track both physical and emotional responses can aid in refining the fasting regimen. With proper guidance and awareness, intermittent fasting can become a valuable tool for individuals aiming to manage inflammation actively.
As research into intermittent fasting continues to expand, a future rich in possibilities beckons. The interest shown by the scientific community suggests that we will gain deeper insights into how fasting affects inflammation in various populations. Investigators are keen to explore cellular mechanisms and how long-term adherence to fasting influences inflammatory markers systematically. Also, the integration of technological advancements, such as wearable health trackers and mobile health applications, can facilitate real-time monitoring of health outcomes, leading to personalized fasting protocols. With growing public interest in holistic health approaches, intermittent fasting could bridge the gap between traditional dietary guidelines and innovative health strategies. Consequently, educational initiatives might emerge, equipping patients and healthcare providers alike with the knowledge necessary to implement effective fasting regimes. Additionally, potential collaborations between researchers and healthcare professionals can ensure that findings are translated into practical recommendations. As the body of knowledge regarding IF and inflammation management grows, it will undoubtedly contribute to enhanced health policies and individualized health plans that prioritize inflammation reduction and overall well-being.
Conclusion
In summary, intermittent fasting represents an intriguing frontier in the management of inflammation. Emerging evidence indicates a promising relationship between intermittent fasting and inflammation reduction, potentially offering a complementary approach to traditional treatments. As ongoing studies delve into the specific mechanisms at play, practitioners are encouraged to consider IF as a viable option in inflammation management. Understanding biological responses to fasting can lead to better strategies for preventive healthcare, particularly in combating lifestyle-related diseases. For optimal success, further research is essential to unveil the nuances of individual fasting responses, dietary compositions, and long-term adherence strategies. Moreover, establishing a comprehensive framework for healthcare providers to discuss IF with patients is crucial for fostering informed decision-making. If evidence continues to support its benefits, intermittent fasting could become a standard recommendation in dietary guidelines, promoting a culture of health and wellness across diverse populations. Thus, the future of intermittent fasting research remains bright, filled with the potential to reshape our understanding of dietary approaches in managing inflammation effectively.
Continued research into intermittent fasting will enable revealing crucial connections between dietary practices and cellular health, ultimately enhancing strategies for reducing inflammation. As more individuals gravitate towards IF, its role in the broader scope of health interventions promises to yield significant insights. Sustainability of such dietary practices will likely be influenced by ongoing motivational programs and community engagement that promote wellness. Hence, the evolution of the narrative surrounding intermittent fasting is not just scientific but also a social phenomenon. Collective efforts in the realms of research and practice will be vital to mainstreaming evidence-based approaches that hold potential for managing inflammation. Intermittent fasting may emerge not only as a tool for individual health enhancement but also as a catalyst for broader public health initiatives. The fusion of scientific advancements with practical applications in daily life may lead to a new paradigm in health management strategies. The journey ahead is full of promising discoveries, poised to empower individuals to take control of their health and manage inflammation effectively through informed dietary choices.